A 59-year-old woman with rheumatoid arthritis (RA) presented to our pulmonary clinic for progressively worsening dyspnea of five years’ duration. She described progressively worsening dyspnea after a few minutes of walking on level ground. In addition, she noted worsening pain and morning stiffness of the wrists, knees and metacarpophalangeal (MCP) joints, with subcutaneous nodules. She denied fever, weight loss, cough, chest pain, palpitations and orthopnea.
She was diagnosed with RA seven years earlier and initially treated with prednisone, followed by adalimumab and methotrexate. Subsequently, her therapy was changed to tocilizumab monotherapy, which had been administered for the prior four years.
Four years before presenting to our clinic, she had also been diagnosed with chronic obstructive pulmonary disease (COPD) on the basis of abnormal pulmonary function tests. She had a five pack-year smoking history, but had quit smoking more than 20 years before. For the COPD, she was treated with inhaled tiotropium, fluticasone/salmeterol and albuterol, but experienced little symptomatic relief.
An examination revealed bilateral, faint inspiratory crackles with no wheezes or rhonchi. The musculoskeletal exam was remarkable for warm, tender and boggy wrists, MCP and knee joints. A serologic evaluation was initiated, and 40 mg of prednisone daily was started.
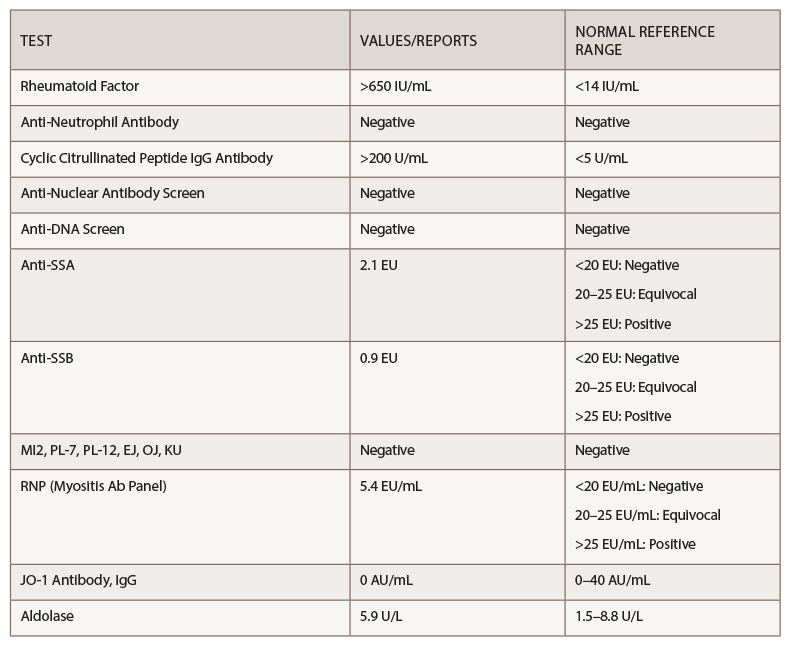
Her rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) were above the level of detection, at >650 IU/mL and >200 U/mL, respectively (see Table 1).
Pulmonary function testing revealed severe airway obstruction with no response to bronchodilators, markedly increased residual volume, suggestive of significant air trapping, and relatively preserved diffusion capacity for carbon monoxide (DLCO) (see Figures 1A and B, below). High-resolution computed tomography (HRCT) lung scanning with expiratory imaging revealed hyperinflation, diffuse bronchial thickening and mosaic attenuation in the areas of airway abnormality suggesting air trapping (see Figures 2A and B). She was subsequently diagnosed with obliterative bronchiolitis associated with RA (OB-RA).
Discussion
Epidemiology: RA is a common systemic inflammatory disorder of unknown etiology with a prevalence of about 1% of the general population.1 Extra-articular manifestations are common, leading to progressive disability, and are associated with increased mortality and socioeconomic costs. Pulmonary complications of RA are numerous and include interstitial lung disease, bronchiectasis/chronic bronchitis, pulmonary vasculitis, necrobiotic lung nodules and pleural effusion/fibrosis. Together, these are a significant cause of death in patients with RA.2,3
Obliterative bronchiolitis (OB), also known as bronchiolitis obliterans or constrictive bronchiolitis, is a rare pulmonary manifestation of RA presenting as severe obstructive small-airway disease. The occurrence of OB is not unique to RA and has been found in various clinical settings, including toxic inhalation, Sjögren’s syndrome, and following pulmonary and stem cell transplantation, suggesting OB is a final common pathway of airway destruction rather than a distinct clinical entity.4
OB following transplantation (OB-transplant) has been the subject of considerable study, but knowledge about OB in non-transplant patients remains limited. Obliterative bronchiolitis in patients with RA was first reported by Geddes et al. in 1977, with subsequently published literature about this entity being predominantly individual case reports and case series.5