AURORA 2
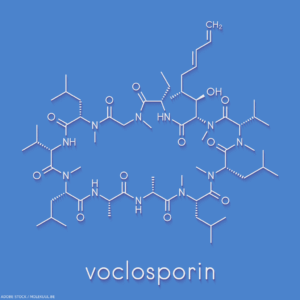 Voclosporin, a novel calcineurin inhibitor (CNI), is associated with a favorable metabolic profile with regard to lipids and glucose, and a predictable pharmacokinetic profile, resulting in no need for the therapeutic drug monitoring required of other CNIs. AURORA 2, a double-blind, phase 3 study, evaluated the longterm safety, tolerability and efficacy of voclosporin compared with placebo in patients with lupus nephritis receiving an additional two years of treatment following completion of the one-year AURORA 1 study.
Voclosporin, a novel calcineurin inhibitor (CNI), is associated with a favorable metabolic profile with regard to lipids and glucose, and a predictable pharmacokinetic profile, resulting in no need for the therapeutic drug monitoring required of other CNIs. AURORA 2, a double-blind, phase 3 study, evaluated the longterm safety, tolerability and efficacy of voclosporin compared with placebo in patients with lupus nephritis receiving an additional two years of treatment following completion of the one-year AURORA 1 study.
Methods: Patients enrolled in AURORA 2 continued on the same treatment randomly assigned in AURORA 1, in combination with mycophenolate mofetil and low-dose glucocorticoids. Safety evaluation included assessments of adverse events and biochemical and hematological laboratory assessments during the study. Efficacy was assessed by achievement of complete renal response and partial renal response, good renal outcome, renal and non-renal flare, and changes in urine protein creatinine ratio, estimated glomerular filtration rate (GFR) and serum creatinine.
Results: Two hundred and sixteen patients were enrolled in AURORA 2. Treatment was well tolerated, with 86.1% of participants completing the study and no unexpected safety signals. Adverse events occurred in 86% of patients in the voclosporin group and 80% of patients in the control group, with an adverse event profile similar to that seen in AURORA 1, albeit with reduced frequency. Adverse events of both GFR decrease and hypertension occurred more frequently in the voclosporin group than in the control group. Mean corrected estimated GFR was within the normal range and stable in both treatment groups. Improved proteinuria persisted across three years of treatment, leading to more frequent complete renal responses in patients treated with voclosporin.
Conclusion: Data demonstrate the safety and efficacy of long-term voclosporin treatment over three years of follow-up in patients with lupus nephritis. Overall, three-year data provide further support for the use of voclosporin with mycophenolate mofetil and low-dose glucocorticoids for the treatment of lupus nephritis.
Excerpted & Adapted From
Saxena A, Ginzler EM, Gibson K, et al. Safety and efficacy of long-term voclosporin treatment for lupus nephritis in the phase 3 AURORA 2 clinical trial. Arthritis Rheumatol. 2024 Jan;76(1):59–67.
Note: For source material, refer to the full study.
Urinary Biomarkers
Renal biopsy remains the gold standard for the definitive diagnosis and classification of lupus nephritis. But it is an invasive procedure accompanied by bleeding to various degrees and is not feasible in cases with associated complications and risk factors. Therefore, the development of noninvasive, predictive biomarkers for renal histopathological findings is needed.
This study aimed to identify the pathogenic signal pathway and elucidate urinary biomarkers for predicting the presence or severity of histologic findings in lupus nephritis.1
Methods: Urine samples from patients with biopsy-proven active lupus nephritis were screened for 1,305 proteins using an aptamer-based proteomic assay. The diversity and expansion of individual renal histologic features in lupus nephritis were quantified to identify the urinary proteins associated with the histologic findings found in each score. Candidate urinary proteins were validated in a validation cohort. Immunohistochemical staining of the renal tissues was performed to clarify the localization of the candidate proteins.
Results: Cluster analysis extracted five histologic subgroups according to their correlations with each histologic finding in lupus nephritis. Protein groups that correlated with each histologic subgroup revealed a distinct pathogenesis in lupus nephritis using pathway analyses. Enzyme-linked immunosorbent assay validation revealed that urinary calgranulin B (S100A9), monocyte chemotactic protein 1 (MCP-1), and insulin-like growth factor binding protein 5 (IGFBP-5) levels could specifically predict the presence and severity of active glomerular lesions, interstitial inflammation, and interstitial fibrosis, respectively. Immunohistochemical staining revealed the localization of these proteins in each lesion.
Commentary: “Although this study involved a relatively small sample size, it lays promising groundwork for the conceptualization of a liquid biopsy in [lupus nephritis],” wrote Andrea Fava, MD, Johns Hopkins University, Baltimore, in a commentary in the same issue of Arthritis & Rheumagology.2 “Biomarkers, by definition, provide a more convenient or noninvasive way [than kidney biopsy] to reflect biologic states or predict outcomes. … The framework proposed by this study, with its focus on principal histologic components and their relative biomarkers, might, if validated, refine the current prognostic limitations of renal biopsies by introducing a granular, longitudinal perspective through noninvasive biomarkers.”
Excerpted & Adapted From
- Hiramoto K, Saito S, Hanaoka H, et al. Urinary biomarkers associated with pathogenic pathways reflecting histologic findings in lupus nephritis. Arthritis Rheumatol. 2025 Mar;77(3):298–310.
- Fava A. Urinary biomarkers: Toward a liquid biopsy for lupus nephritis. Arthritis Rheumatol. 2025 Mar;77(3):244–246.
Note: For source material, refer to the full study.



