Referral triage, primary care resources & smarter screening strategies
CHICAGO—In a session at ACR Convergence 2025, three speakers discussed novel strategies practices can implement to better triage patients and provide improved access to rheumatology care.
Improving Access to Care
Jay Doss, MD, associate professor of medicine and clinical vice chief of the Division of Rheumatology at Duke University School of Medicine, began by reviewing strategies to improve referral triage and the use of e-consults.
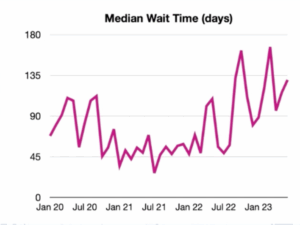
He explained how, with ballooning wait times across rheumatology practices nationally, an increasing need exists to be more selective about the patients accepted to be seen in clinic. Data for rheumatology clinics at Duke University shows median wait times have increased to 160 days as of 2023 (Figure 1, below).
Additionally, the longer the wait time, the higher percentage of patients who will no show or not attend the visit. The no-show rate is around 15% for patients scheduled within 90 days, but doubles to 30% for patients waiting nine to 12 months for an appointment.
“Every no show for a new patient is a missed opportunity for a patient who needs our care,” Dr. Doss said.
Referral Triage
To address these challenges, many institutions are using referral triage, a process in which incoming referrals are reviewed, and appointments are preferentially allocated to patients with a higher likelihood of rheumatic disease.
“Many practices are restricting appointments for certain referrals, such as fibromyalgia, osteoarthritis, hypermobility or chronic fatigue,” Dr. Doss said.
Potential challenges for referral review include missing patients with real rheumatic disease, disgruntled patients or referring clinicians, and time necessary for manually reviewing charts.
Benefits of E-Consults
Another modality of providing access to care are e-consults, which are asynchronous, non-patient facing communications between healthcare providers giving diagnostic and/or treatment recommendations to referring clinicians.
The process first involves a referring provider placing an e-consult order—for example—for a patient with a positive antinuclear antibodies (ANA) test. The rheumatologist will then perform a medical record review, provide diagnostic and/or treatment recommendations, and accept or decline an in-person appointment.
“E-consults have many benefits, including screening out low yield referrals, expediting urgent appointments, and educating referring providers,” Dr. Doss said. “Primary care providers have also learned over time from reading e-consult recommendations, and now, they are more likely to complete some of the initial workup on their own.”