Vasculitis is a group of chronic inflammatory diseases in which the blood vessel is the target of an immune reaction. They can be secondary to connective tissue disease, idiopathic or due to infection, neoplasm or drugs.1 Primary angiitis of the central nervous system (PACNS) is a rare syndrome characterized by inflammatory cell infiltration and necrosis of small- and medium-sized blood vessels of the brain parenchyma, spinal cord and leptomeninges.2 It was reported in 1922 by Harbitz as an unusual type of arteritis associated with multinucleate giant cell arteritis of the small meninges and cerebrum and was first reported as a distinct clinical-pathologic entity in an article by Cravioto and Feigin in 1959.3,4
The estimated annual incidence rate of PACNS is 2.4 cases per 1 million person-years. Middle-aged men are most often affected by PACNS, with a median age at onset of approximately 50 years and a male-to-female ratio of approximately 2:1.5 We describe the clinical, imaging and histopathological findings in a patient with PACNS.
Case Presentation
A 37-year-old woman presented at the emergency department with altered mental status, bilateral vision loss and weakness. She had a past medical history significant for multiple sclerosis on interferon beta, type 1 diabetes, hypertension, stage 4 chronic kidney disease and vitamin D deficiency. The patient was in her usual state of health on the morning of presentation.
Around 7:30 a.m. she held a phone conversation with her father who had traveled to her home to transport her to a previously scheduled doctor’s appointment. She did not answer the door, but her father could hear her fumbling with the lock. He contacted the property manager and gained access to the home at approximately 8:45 a.m. At that time, he found her standing at the doorway, confused. When he questioned his daughter, she replied in streams of unintelligible, mumbled speech. Her father helped her to a couch and noted she had a poorly coordinated gait.
Based on her symptoms, her father took her to the emergency department for evaluation. The patient had no recollection of the morning’s events and reported regaining her orientation and awareness on the way to the hospital.
On arrival at the emergency department, she was afebrile and tachycardic (HR 100 beats per minute), with a blood pressure of 125/75 mmHG. She was breathing normally, with oxygen saturation of 99% on room air.
When the patient was admitted to the medical ward, her vision loss had resolved. The physical exam was notable for normal mental status, right upper extremity mild dysmetria, with 4/5 strength in the right upper extremity and right lower extremity, with normal sensation and tone. There was no evidence of meningitis or focal neurologic signs.
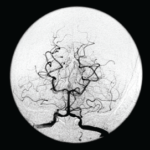
Imaging was obtained and included a computed tomography (CT) of her head, which showed several lesions suspicious for acute or subacute infarction.
Magnetic resonance imaging (MRI) of her brain showed widespread foci of restricted diffusion with corresponding low apparent diffusion coefficient (ADC) signal throughout both cerebral and cerebellar hemispheres, most suggestive of acute infarcts. The distribution was atypical for multiple sclerosis, so they were not thought to be demyelinating plaques, despite her past history. Scattered T2/FLAIR signal hyperintensities noted within the left cerebellum and right cerebral peduncle were suggestive of remote infarcts (see Figures 1 and 2).