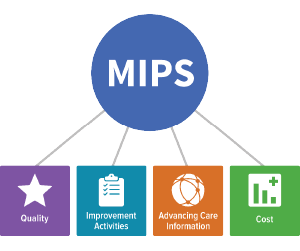
You can now use the updated Centers for Medicare & Medicaid Services (CMS) MIPS Participation Lookup Tool to check on your 2018 eligibility for the Merit-Based Incentive Payment System (MIPS). Enter your National Provider Identifier (NPI) in the tool to find out whether you need to participate during the 2018 performance year.
Changes to Low-Volume Threshold
 To reduce the burden on small practices—and in response to advocacy from the ACR, the American Medical Association and others—the CMS changed the eligibility threshold for 2018. Clinicians and groups are now excluded from MIPS if they:
To reduce the burden on small practices—and in response to advocacy from the ACR, the American Medical Association and others—the CMS changed the eligibility threshold for 2018. Clinicians and groups are now excluded from MIPS if they:
- Billed $90,000 or less in Medicare Part B-allowed charges for covered professional services under the Physician Fee Schedule (PFS) from Sept. 1, 2016, to Aug. 31, 2017; or
- Provided professional services under the PFS to 200 or fewer Medicare Part B-enrolled beneficiaries from Sept. 1, 2016, to Aug. 31, 2017.
This means that to be included in MIPS for the 2018 performance period, you need to have billed more than $90,000 in Medicare Part B-allowed charges for covered professional services under the PFS and have furnished covered professional services under the PFS to more than 200 Medicare Part B-enrolled beneficiaries from Sept. 1, 2016, to Aug. 31, 2017. Note: The 2018 Participation Lookup Tool Update for Alternative Payment Model (APM) participants will be updated at a later time.
Find Out Today
Find out whether you’re eligible for MIPS today. Prepare snow to earn a positive payment adjustment in 2020 for your 2018 performance.
