-
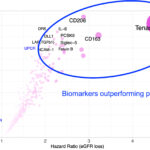
- Figure 1: Urinary Tenascin C, & Other Urinary Biomarkers at 12 Months, Predicts Future Kidney Function Loss in Lupus Nephritis, & Outperform Proteinuria. Source: Dr. Andrea Fava
-
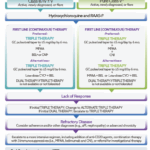
- Figure 2: 2024 ACR Lupus Nephritis Guideline—Treatment Overview. Source: American College of Rheumatology
“Since these urinary biomarkers parallel intrarenal inflammation and predict future GFR, they could detect early treatment responses or failures, and in a few years, allow us to make earlier treatment changes in nephritis patients more precisely,” Dr. Fava said. “This can help inform tapering of immunosuppression, serve as surrogate endpoints in clinical trials and better identify lupus nephritis before proteinuria.”
Approach to Patients with Inadequate Response
Next, Maria Dall’Era, MD, Jean S. Engleman Distinguished Professor of Medicine and chief of the Division of Rheumatology at the University of California, San Francisco, presented an approach on how to apply the 2024 ACR Lupus Nephritis Guideline to patients who experience an inadequate response to treatment or have refractory lupus nephritis.
The guideline defines inadequate renal response as no complete response or partial response by 6–12 months. Refractory lupus nephritis is defined as failing two different, appropriate, six-month therapy courses.6
Dr. Dall’Era reviewed a checklist of key considerations when encountering patients with lupus nephritis with inadequate response. These include assessing adherence (i.e., therapeutic drug level monitoring), confirming appropriate dosing, confirming accuracy of the UPCR, assess for non-immunologic mechanisms and consider alternative diagnoses or repeat kidney biopsy.
“Medication dose and patient adherence should be assessed regularly throughout treatment, particularly as an important first step in evaluating inadequate response or refractory lupus nephritis,” Dr. Dall’Era said.
Non-immunologic mechanisms that can cause ongoing proteinuria due to hyperfiltration or CKD progression include high salt intake, being overweight, hypertension and high protein diet. “Your patient might have an increased level of proteinuria due to hyperfiltration from a high salt meal the night before,” she said.
A repeat kidney biopsy can also be informative, particularly to exclude alternative etiologies of kidney dysfunction, such as thrombotic microangiopathy, other vascular lesions (arteriosclerosis), aPL nephropathy, lupus podocytopathy or fibrosis or chronicity without ongoing activity. Repeat kidney biopsy can be considered if there is partial response, a presumptive flare, CKD progression, or prior to withdrawal of immunosuppression.7
Dr. Dall’Era also mentioned complement-mediated thrombotic microangiopathy (TMA), formerly termed atypical hemolytic uremic syndrome. “It is important to recognize, as it is being increasingly diagnosed amongst our patients with SLE— and it requires anti-complement therapy in addition to standard therapies for SLE,” she said.