The Criteria: Approach & Results
With this goal in mind, the expert committee pooled 10 different prospective, observational cohorts of people with arthralgias at risk for RA. None of the participants had clinically apparent inflammatory arthritis at the start of their respective studies. This specific pooled dataset and analysis also did not include patients who lacked symptoms of arthralgia but had other risk factors for RA. The pooled cohort, with data gathered from the Netherlands, Germany, Italy, Austria and the U.K., ultimately included almost 2,300 people.1
The primary end point was clinically apparent inflammatory arthritis in one or more joints, identified by physical exam. Dr. Deane points out that most rheumatologists would begin treatment for such patients if they saw them in clinic. Although this end point was technically defined in terms of inflammatory arthritis, due to inadequate study information to meet full classification criteria for RA in some cohorts, it’s assumed the majority would also clinically classify as having RA. Moreover, a second analysis with RA as an end point showed similar accuracy.
Ultimately, the main analysis included 24 potential clinical variables and serologic variables, although not every single variable was available in each individual—a challenge in combining cohort data. The team created a logistic regression model and a risk stratification model using the 24 clinical and serological variables and the primary end point outcome.
They used these findings to create a stratification method using six clinical and serological variables found to be strongly associated with the development of inflammatory arthritis. These were:
- Difficulty making a fist;
- Patient-reported morning stiffness;
- Patient-reported joint swelling;
- Increased C-reactive protein;
- Positive rheumatoid factor; and
- ACPA positivity.
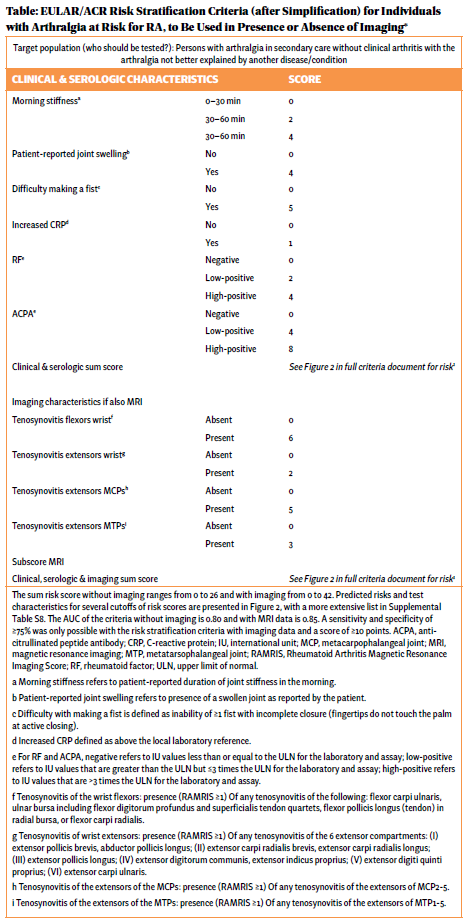
Based on their respective predictive power, these were given different weights (e.g., four points for patient-reported joint swelling, five for difficulty making a fist, four points for low but positive ACPA, eight points for high-positive ACPA (see Table).
The team also analyzed 10 ultrasound and 12 magnetic resonance imaging (MRI) variables, to see if imaging could improve discriminatory ability. Their specific analysis did not find that ultrasound further enhanced detection, but adding MRI improved the ability to accurately predict inflammatory arthritis.
Thus, a patient’s risk stratification criteria can be assessed just using clinical and serological parameters (with risk scores ranging from 0 to 26). Alternatively, adding additional MRI criteria, where available, can further improve accuracy (risk scores ranging from 0 to 42).