The Physician Quality Reporting Initiative (PRQI) is a voluntary quality reporting program initiated by the Centers for Medicare and Medicaid Services (CMS) in 2007. CMS provides bonus payments to eligible providers who successfully report on applicable PQRI measures. For 2010, rheumatologists who successfully participate in PQRI can earn an incentive payment of 2% of the total Medicare Physician Fee Schedule–allowed charges for services provided during the 2010 reporting period. Here are answers to some of the most common questions regarding PRQI.
Am I Eligible, and Where Do I Sign Up?
Most rheumatology providers who are paid under the Medicare fee schedule meet the ”Eligible Provider” definition and qualify to participate in PQRI, including nonphysician providers such as physician’s assistants and nurse practitioners. For a list of providers eligible to participate in the PQRI program, visit www.cms.gov/pqri. Registration with CMS is not required to participate in the PQRI program.
How Do I Get Started?
There are two mechanisms for submission, multiple reporting options, variances in measures to be reported, and a timeframe for reporting. To start, first choose your reporting mechanism, then what measures you will report on, and lastly, a timeframe to submit quality data.
Reporting Mechanism
Providers have the option of reporting PQRI measures through claims or through a qualified PQRI registry.
Claims Based
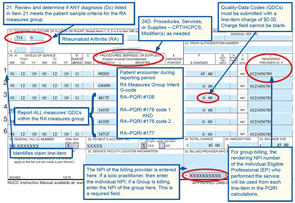
To report PQRI through claims submitted to CMS, the provider will add a CPT II code to an appropriate patient encounter/claim. An appropriate claim includes the CPT code, ICD-9 code, and any other codes included in the denominator of the PQRI measure. The CPT II code is a five-digit alphanumeric code used to report that an action has been taken, or not taken, to satisfy a measure.
As with CPT coding, there are modifiers to be used in conjunction with the CPT II codes for some of the PQRI measures. These modifier codes are intended to capture valid reasons why an action was not taken.
Remember, the PQRI bonus payments are based on participation, not performance; using the proper modifier codes will ensure that your reporting is accurate.
- 1P exclusion modifier due to medical reasons
- 2P exclusion modifier due to patient reasons
- 3P exclusion modifier due to system reasons
In addition, CPT II codes for PQRI reporting have a modifier to signify that the recommended action was not taken, without a valid reason documented:
- 8P reporting modifier—action not performed, reason not otherwise specified
Reporting the 8P modifier if the action was not taken is important to ensure successful PQRI reporting.
If the provider decides to undertake claims-based reporting on a measure group rather than three individual measures, then the CPT II code G8490 (I intend to report the Rheumatoid Arthritis Measures Group) must be reported on the first claim to notify Medicare that the provider is reporting on a measure group. It is not necessary to submit this initiation code more than once.
For the claims submitted representing patients in which all quality actions for the applicable measures group have been performed, the provider may report one single code, G8499, to signify that all of the measures have been completed in lieu of individual CPT II codes for each measure within the group.
It is important that providers work with practice staff to ensure that appropriate PQRI measure codes are applied to submitted claims because CMS does not offer the opportunity to correct missed PQRI reporting (CPT II code). If a claim is submitted with an incorrect or omitted PQRI reporting code, the encounter will be counted as an unsuccessful attempt to report. Practice workflow should accommodate checks to ensure that claims for patients who meet reporting criteria contain both the CPT code and the appropriate CPT II codes on that claim. Providers will receive a remittance advice for claims submitted with CPT II codes with a standard remark code of N365, indicating that the CPT II code was received by CMS and is for reporting purposes only. It is helpful for a practice reporting via claims to keep track of all PQRI cases reported so that claims submitted can be verified against these N365 codes, indicating a successful transfer of reporting data to CMS.
Note that Medicare Part C–Medicare Advantage beneficiaries cannot be included in the population for claims-based reporting of individual measures or measure groups, but they may be included in the registry-based reporting of measure groups.
Visit www.rheumatology.org/practice, and click on “Office Support” for PQRI coding instructions and a complete list of applicable codes for the rheumatology practice.
Registry
As an alternative to claims-based reporting, a provider may participate in an approved registry, which will submit PQRI quality-measure results and numerator/denominator data to CMS on the provider’s behalf. Registry reporting eliminates the need to submit CPT II codes through claims. A list of qualified registries for 2010 PQRI can be found on the CMS PQRI Web page titled, “Qualified Registries for 2010 PQRI Reporting.”
There are several benefits of reporting via registry.
- First and foremost, the success rate for registry reporting is generally much higher than claims reporting—the success rate in 2008 was 96%.
- Registries provide data quality checks to ensure that all submissions are accurate and complete to avoid rejected measurements.
- The ability to enter and view this data at any point throughout the reporting year means that data entry or chart review can be performed retrospectively in a batch format.
- Most registries will allow you to submit your 2010 data right up until the CMS deadline in late February 2011, eliminating the need to track claims throughout the year. If it’s decided late in 2010 to report PQRI data for the past year, it can be done through a registry. This is not so with claims-based reporting.
- Finally, registries often provide more timely access to data and analyzed reports, which can contribute significantly to practice improvement efforts.
The ACR’s clinical quality registry, the Rheumatology Clinical Registry (RCR), is approved by CMS for PQRI reporting. Through the RCR, ACR members and their staff can submit quality data on the RA measures group for the required 30 patients. For more information on the RCR, visit www.rheumatology.org/rcr.
Measures to Be Reported
Providers can choose to report on either three individual measures or a single measures group.
There are 20 PQRI measures out of the 175 total measures that pertain specifically to rheumatology. Within those 20 measures are two measure groups: the RA measure group that includes six measures and the back pain measure group that includes four.
Providers who choose to report individual measures for PQRI must select at least three measures to report on and must report those measures for at least 80% of applicable patients. “Applicable patients” are those for whom claims are submitted to CMS that include the measure denominator codes.
Providers who choose to report measure groups must report all of the measures in the group for each patient; however, measure-group reporting provides the possibility of reporting on a predictable, defined number of patients. Therefore, measure-group reporting is often considered less burdensome. A list of 20 measures and groups most relevant to rheumatology can be found at www.rheumatology.org/practice; there is also guidance on how to read and interpret the PQRI measure specifications.
Time Frame for Reporting
The PQRI program offers two different reporting periods; the provider must select a period and successfully complete the reporting requirements during that period. Table 1 provides an overview of PQRI reporting requirements for 6-month and 12-month reporting.
Payment
A qualified provider that successfully reports on PQRI measures can receive incentive payments of 2% of the total Medicare Physician Fee Schedule–allowed charges for services provided during the 2010 reporting period.
Incentive payments are available for successful PQRI reporting for up to four years, ending in 2015. If you participate, CMS will issue a feedback report stating whether or not an incentive was earned. However, reports will not provide claim-level details. Beginning in 2015, providers who are not successfully participating in PQRI will incur a negative Medicare payment adjustment of –1.5% for their covered services.
Does the ACR Have Resources to Help?
Providers and practices that are organized and determined can benefit from the self-assessment and bonus payments included in the PQRI program. The ACR offers numerous resources to support your practice as you engage in the PQRI reporting process.
Visit www.rheumatology.org/practice and click on “Office Support,” or contact ACR staff at (404) 633-3777 with questions about PQRI and how your practice can successfully report and attain the 2% incentive payment.
Don’t forget to check out this month’s Coding Corner for a PQRI measure coding example!

