The major strengths of the study are the rigor applied to excluding IBM and the efforts expended to both diagnose and distinguish between dermatomyositis and polymyositis utilizing muscle biopsy, clinical features, and autoantibody analysis. There is sufficient follow-up (only 13% not evaluated at follow-up). This study reflects a tremendous amount of work and effort, although it is retrospective in design and the classification of myositis disease subsets (although previously published) has not been subjected to critical analysis.
In this study, the prognostic factors assessed were age at onset of disease, gender, myositis classification, time to treatment, and presence of myositis-specific autoantibodies. There is a notable absence of organ system involvement among factors evaluated.
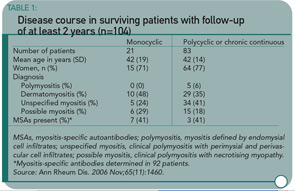
This study confirms that 1) polymyositis and dermatomyositis are serious diseases with a significant mortality rate (>10%) that is highest among those individuals with an underlying malignancy; 2) most myositis patients experience a chronic, continuous disease course (see Table 1), and 3) patients subsequently report high rates of disability and a low quality of life.
The finding that disease classification by muscle biopsy and autoantibody doesn’t affect prognosis is surprising and provocative. However, for me, there are a number of questions still unanswered. I’d like to see this study reanalyzed to include an evaluation of organ involvement (even if it is done retrospectively). Or, better yet, I would like to see a larger cohort study utilizing muscle biopsy, autoantibody, and organ system involvement while adjusting for treatment. If either of these analyses is done, I think the results could affect management of patients with inflammatory myopathy. Identification of true prognostic factors could enable us to identify patients at risk for a poor outcome and consider aggressive treatment to include immunosuppressive agents early in the disease course for these individuals. This would be a true step forward and allow us to begin limiting the mortality and disability from this disease.
Guided Imagery with Relaxation Can Decrease Disability in OA
By Gail C. Davis, RN, EdD
Baird CL, Sands LP. Effect of guided imagery with relaxation on health-related quality of life in older women with osteoarthritis. Res Nurs Health. 2006; 29:442-451.
Abstract
OA is the most common cause of disability in older adults, which, in turn, leads to poor quality of life (QOL). Disability is caused primarily by the joint degeneration and pain associated with OA. A randomized pilot study was conducted to test the effectiveness of guided imagery with relaxation (GIR) to improve health-related QOL (HRQOL) in women with OA. A two-group (intervention versus control) longitudinal design was used to determine whether GIR leads to better HRQOL in these individuals and whether improvement in HRQOL could be attributed to intervention-associated improvements in pain and mobility. Twenty-eight women were randomized to either the GIR intervention or the control intervention group. Using GIR for 12 weeks significantly increased women’s HRQOL in comparison to women who used the control intervention, even after statistically adjusting for changes in pain and mobility. These findings suggest that the effects of GIR on HRQOL are not limited to improvements in pain and mobility. GIR may be an easy-to-use self-management intervention to improve the QOL of older adults with OA.
Commentary
The changes that occur with aging affect both the medications and amount of medication that can be tolerated by older adults, putting them at higher risk for adverse effects. Pharmacokinetic responses, like decreased renal excretion of drugs and changes in drug absorption, and issues related to possible drug interactions and the effects of drugs on the gastrointestinal system present important considerations for the older adult’s management of chronic pain and related QOL. These issues emphasize the importance of this study that tests a non-pharmacological approach, not frequently used by older adults, for improving QOL.