Moyamoya, meaning a “hazy puff of smoke” in Japanese, is a chronic, occlusive cerebrovascular disease involving bilateral stenosis or occlusion of the terminal portion of the internal carotid arteries (ICA) and/or the proximal portions of the anterior cerebral arteries (ACA) and middle cerebral arteries (MCA) that leads to neurological deficits.
Epidemiology
CNS vasculitis was first seen and described from autopsy results in the 1950s and, at that time, was described as granulomatous angiitis. Recent estimates indicate that the annual incidence of PACNS is around 2.4 per million people. Although it has been reported in both children and adults, it is more commonly seen in men from 30–50 years old.1
Moyamoya disease was first described in Japanese literature in 1957 by Takaku and Suzuki.2 It is most commonly found in Asian populations. The incidence of moyamoya disease is highest in Japan with approximately three cases per 100,000 persons, which is 30–40 times higher than in the U.S., where the incidence is approximately 0.086 cases per 100,000 persons. Unlike in PACNS, moyamoya disease is more common in females, with the peak ages of incidence in children at 5 years old and adults in their 40s.3
Clinical Presentation
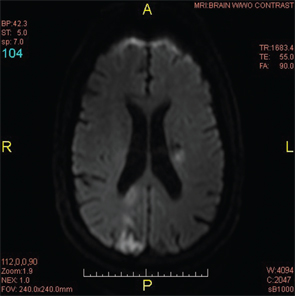
Figure 4: A repeat MRI of the brain two weeks after the initial MRI revealed a new lacunar infarct of the left corona radiata and the old infarct in the right posterior occipito-parietal lobe.
PACNS often has a long prodromal period and is thought to rarely present with acute manifestations. In a review of 116 patients, 83% presented with a change in mental status, 56% with headaches, 30% with seizures, 14% with stroke and 12% with cerebral hemorrhage.4
Clinical presentation of moyamoya disease differs between adults and children. Adults typically present with transient or permanent cerebral infarction and intracranial hemorrhage; however, children present mainly with ischemic events. Although patients can present without any symptoms, patients more often will present with visual deficits, speech disturbances, headaches, intellectual deterioration, cranial nerve palsies and/or gait disturbances.3
Diagnosis
In PACNS, 80–90% of patients have abnormal CSF findings characterized by elevated total protein concentrations.7 Inflammatory markers, such as ESR and CRP, are typically normal, as are ANCA and ANA.
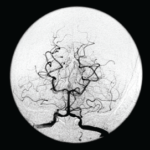
Although imaging of the head is usually nonspecific, the most common findings are infarcts. The infarcts can involve any part of the subcortical white matter, deep gray matter, deep white matter or the cerebral cortex. Angiography is often used as a diagnostic test, although its specificity and sensitivity are very low and, therefore, cannot be used as a sole determinant of the etiology of the patient’s symptoms. Typical findings, however, include alternating areas of narrowing and dilation of the arteries, which can give the vessels a beaded appearance. Other diagnostic features include arterial occlusion of many cerebral arteries without atherosclerosis or other abnormalities, but in the end, the gold standard for diagnosis of PACNS continues to be a brain biopsy. Histopathology will often show either a granulomatous, lymphocytic or necrotizing vasculitis.3