CHICAGO—During a session of ACR Convergence 2025, speakers discussed intriguing possibilities about the role of the gut microbiome in the development of rheumatoid arthritis (RA), as well as its potential impacts in treatment response to methotrexate.
The Microbiome’s Multifaceted Role
Researchers are actively exploring how the microbiome impacts such conditions as respiratory disease, diabetes, inflammatory bowel disease, heart disease, cancer, liver and kidney diseases, and brain disorders.1 In rheumatology, scientists have identified modifications of the microbiome in conditions such as systemic lupus erythematosus, systemic sclerosis, Sjögren’s disease and RA, although the exact implications of these differences are a matter of ongoing research.2
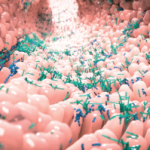
One of the speakers was Christopher Rooney, MD, PhD, MRCP, a clinical lecturer in medical microbiology at the University of Leeds in England. He noted the human body is a complex ecosystem, with roughly 500–1,000 different species of bacterial cells existing in a roughly 1:1 ratio to human cells. The complete microbiome consists of a variety of bacteria, viruses, fungi and archaea, but bacteria in the gut are the largest and most metabolically active component, and they are the primary topic of current scientific investigations.3
Among different individuals, the microbiome is remarkably varied. Diet plays a major role in its composition, as do other elements, such as smoking and various diseases and medications. However, these known factors account for only a minority of this variability, noted Dr. Rooney.4
Finding ways to quantify patterns and differences in the microbiome is a major research challenge given the dynamic complexity of the environment, necessitating sophisticated statistical and computational analyses. Researchers can characterize the specific species present, their abundance, their genomics and their metabolic activity.3
The microbiome plays many important roles, such as aiding digestion and preventing infection, but for autoimmune conditions, its role in immune homeostasis may be key.
Another speaker, rheumatologist Renuka Nayak, MD, PhD, explained, “Our immune system relies on the microbiome for its own education on [self] tolerance, and for the development of a lot of immune cell populations.” Dr. Nayak is an associate professor of medicine at the University of California, San Francisco.
“The gut microbiome is in constant conversation with the immune system,” agreed Dr. Rooney. “The breakdown of that dialogue can lead to the breakdown of immunological tolerance.”
The Gut & Methotrexate
The burgeoning field of pharmacomicrobiomics, which investigates the effects of the gut microbiome on drug metabolism, has led to important discoveries in HIV and cancer therapies. Dr. Nayak has added to this body of research through detailed work studying the impact of the microbiome on responsiveness to methotrexate in people with RA.5-8