Although it is first-line treatment for RA, more than 50% of patients inadequately respond to oral methotrexate as monotherapy, noted Dr. Nayak, and no current biomarkers can reliably predict response.9 Current guidelines from the ACR recommend maximizing methotrexate before moving to other therapies for RA.10
“A current, unmet need is to quickly identify patients who are not going to be optimally responsive to methotrexate,” said Dr. Nayak. This would allow clinicians to escalate therapy and potentially control disease more quickly and perhaps more effectively long term.
Dr. Nayak found pretreatment gut microbiome diversity differed significantly in newly diagnosed RA patients who went on to become methotrexate responders compared to patients with inadequate response to the drug. Using a machine learning program, the research team could even predict treatment response in a majority of patients using their initial microbiome data, outperforming current clinical and pharmacogenetic markers.5
In ex vivo studies and mouse models, they also explored how microbiome bacteria from non-responders tend to metabolize more methotrexate and decrease levels of methotrexate more rapidly than responders. Methotrexate metabolites produced by gut microbial communities may also contribute to variation in treatment response, and these may prove useful tools in predicting who will respond to methotrexate therapy.5-8
“If we understand these mechanisms and can shift the chemical equilibrium away from methotrexate metabolism, that may be another opportunity to maximize methotrexate efficacy and improve care for our patients,” said Dr. Nayak.
The Gut as a Trigger?
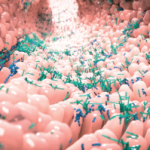
Much of Dr. Rooney’s research centers on the hypothesis that the gut microbiome is a potential trigger for the development of autoimmunity in RA, and thus potentially a modifiable risk factor.
Local changes in the gut mucosal level (e.g., via antigen presentation of molecules produced by bacteria) may cascade through the immune system and lead to systemic effects.3 Dr. Rooney and others have also shown certain microbiome changes may be associated with increased intestinal permeability and positivity for anti-citrullinated protein antibodies (ACPA), a major risk factor for RA.11
The gut microbiome in established RA shows clear evidence of changes, Dr. Rooney said, but it’s less clear exactly what aspects of that microbiome might be pathogenic. He also acknowledged a tension that hasn’t fully been resolved: Elements of the gut microbiome might help drive autoimmunity, or changes in the microbiome might be due to local and systemic inflammation already present.