If CMS wishes to change payment schedule, I think that it should increase the new patient evaluation to the same reimbursement for the work and not use obfuscation to pay less. I think that the amount of effort during consultation is misinterpreted or ignored in a way that payors can use to decrease payments. Reduced reimbursement can directly impair the care of our patients. Regrettably, there is little in the Shalowitz article on the amount of work that was done by the physicians, the complexity of patients involved, and the quality of the work done. Shalowitz proposes that primary care physicians are unfairly treated by consultants. I strongly disagree. I believe that Dr. Shalowitz’s ideas foster unnecessary competition and discord between generalists and specialists and misconstrue the value of the consultation.
Shouldn’t Correct Count?
The best, most cost-effective diagnosis is the correct diagnosis. As a rheumatologist, I have saved patients, Medicare, and insurance companies countless dollars with the correct diagnosis, but nowhere in the Shalowitz article is the quality of the consultation considered. Many of our colleagues have commented on this article on the ACR Advocacy list serve. Paul Rochmis, MD, noted that the author’s statement that cognitive specialists “are paid so much more … or the same for less time spent with [patients]” is patently absurd (January 13, 2010). Where are the data supporting this statement? Does the author—and by extension, the editor—really think that the knowledge and experience in treating complex chronic illnesses will automatically flow from the medical specialist to the primary care physician with the 6% transfer of reimbursement? Chris Morris, MD, suggests Dr. Shalowitz does not understand the financial aspects of a private medical practice (January 13, 2010).
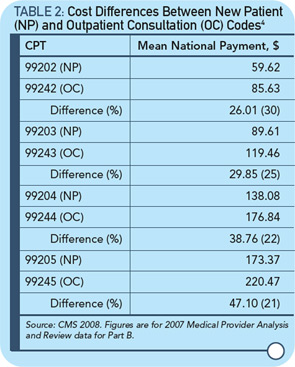
Dr. Shalowitz calculates the savings from this CMS rule change. If we rely on his data, this sum is $534.5 million dollars annually.1 For less than 1% savings, elimination of consultation codes will eliminate many Medicare patients’ access to specialists, as Dr. Rochmis noted on the ACR Advocacy list serve. Meanwhile, Tim Menke, deputy inspector general for investigations at the Department of Health and Human Services, estimates that Medicare fraud costs $60 billion a year and they only retrieve about $4 billion a year.5 Thus, instead of going after those who cheat Medicare, they go after physicians who have honestly worked hard for years for the care of their patients.
