 CHICAGO—At a session of ACR Convergence 2025, attendees explored several topics from the vantage of complementary and alternative medicine, many of which could easily be incorporated into a more traditional medical approach.
CHICAGO—At a session of ACR Convergence 2025, attendees explored several topics from the vantage of complementary and alternative medicine, many of which could easily be incorporated into a more traditional medical approach.
Putting Out the Fire of Inflammation
The speaker, Nisha Manek, MD, FACP, FRCP, is a telemedicine integrative rheumatologist with Avel eCare and is based in Yorba Linda, Calif. She has added to her conventional rheumatology expertise with various kinds of training in complementary medicine, such as through the University of Arizona’s Fellowship in Integrative Medicine.
Dr. Manek urged her colleagues to pursue alternative avenues to “fight the fire” of their patients’ inflammation. She advocated for finding ways to address inflammation at its origin and not just through standard therapies.
Diet
Dr. Manek shared stories of some patients whose symptoms remarkably improved after changing some simple components of their diet. However, she also noted that making big changes can be challenging for patients. “Our patients don’t choose to eat badly. The reality is they’re surrounded by processed foods,” she said. “That’s what’s easy and accessible.”
Simple questions about about diet are not a standard part of the diet are not a standard part of the rheumatology medical history and review of systems, Dr. Manek pointed out; further, taking time to ask such questions may not be billable. “A question like, ‘What did you eat for breakfast today?’ may look deceptively simple, yet it is concrete and modifiable. Find out what your patients are eating,” she urged.
Mediterranean Diet & Ultra-Processed Foods
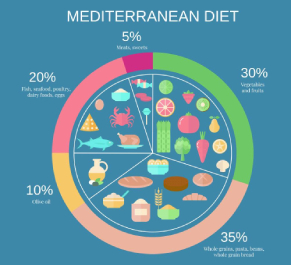 Dr. Manek noted the ACR recommends a Mediterranean diet, which emphasizes intake of vegetables, fruits, whole grains, nuts, seeds and olive oil, with moderate portions of dairy, fish, poultry, eggs and beans. Importantly, the diet also limits added sugars, refined carbohydrates and highly processed foods.1
Dr. Manek noted the ACR recommends a Mediterranean diet, which emphasizes intake of vegetables, fruits, whole grains, nuts, seeds and olive oil, with moderate portions of dairy, fish, poultry, eggs and beans. Importantly, the diet also limits added sugars, refined carbohydrates and highly processed foods.1
Zoning in on this latter category, Dr. Manek especially warned that many foods can contain additives not optimal for controlling inflammation. Such foods are also often high in sugar, fat and salt.
Generally speaking, the rheumatology community agrees that large amounts of highly processed “junk foods” can worsen patients’ health. For example, two recent studies found that ultra-processed foods may increase the risk of rheumatoid arthritis (RA).2,3
Dr. Manek also recommended limiting the use of factory-produced seed oils, such as soybean, corn, cottonseed, canola, grapeseed, sunflower, safflower and generic vegetable oil, usually some blend of these. This is consistent with current health trends positing their role in inflammation, perhaps due to the way these oils are processed or their omega-6 content. Although this is not in line with much of the current expert opinion on the subject, such oils are quite common in ultra-processed foods, so limiting them in that setting may be beneficial.4,5


