This week, the Coalition sent Congressional leadership a letter detailing the results of a recent survey about how underwater biosimilars are impacting physicians’ ability to provide high-quality care. Almost all of the nearly 200 practices queried reported being underwater on several biosimilars, with rituximab and infliximab biosimilars being the most common.
ACR Leaders Discuss Rheumatology Medications at Medicare Drug Price Negotiation Town Hall
On April 30, Rebecca Shepherd, MD, MBA, and Amanda Myers, MD, represented rheumatology in a live town hall on the Medicare Drug Price Negotiation Program, describing the benefits of apremilast and nintedanib for patients with rheumatic disease.
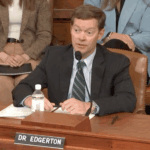
Colin Edgerton, MD, Testifies in Congressional Hearing on Biosimilars
In front of the U.S. House Ways and Means Subcommittee, Dr. Edgerton described how challenges of biosimilar costs threaten patient care and outlined several potential legislative solutions.
March Updates from the ACR Insurance Subcommittee
The Insurance Subcommittee is working on behalf of ACR members to address underwater formulary requirements for biosimilars, mandated switches to biosimilars, evaluation and management downcoding and more.
Will Telehealth Make It to April?
Medicare’s current telehealth flexibilities are set to expire March 31. To avoid a government shutdown, Congress must pass a appropriations package by midnight on March 14. The ACR is preparing for the impacts if a telehealth extension does not pass.

Rheumatologist Elected to Key AMA Committee That Helps CMS Set Medicare Reimbursements
Luke Barré, MD, MPH, RhMSUS, has been elected to the American Medical Association’s Relative Value Update Committee. He is the second rheumatologist to hold the seat in recent years and will ensure representation of the specialty during valuation of physician services.
ACR Comments on Proposed Medicare Advantage Changes
In response to proposed changes to the Medicare Advantage and prescription drug programs for contract year 2026, the ACR submitted comments on the provisions related to the Inflation Reduction Act, prior authorization and the influence that pharmacy benefit managers have on the placement of biosimilars on formularies.

Hit the Ground Running with New Insurance Subcommittee Chair Michael Feely, MD
Dr. Feely discusses his previous work with the College, his current work as a practicing rheumatologist and how he will lead continued advances on the insurance front.
What Providers & Patients Should Know About Medicare Benefit Changes in 2025
Changes to Medicare benefits in 2025 include an annual $2,000 cap on out-of-pocket costs for covered Part D drugs and a new, voluntary Medicare Prescription Payment Plan intended to help beneficiaries manage drug costs.
Resources for Practices to Fight Payer Downcoding of E/M Services
The American Medical Association and ACR Insurance Subcommittee offer support and guidance to help practices recognize and push back against downcoded payments for evaluation and management services.
- « Previous Page
- 1
- 2
- 3
- 4
- …
- 8
- Next Page »