NEW YORK (Reuters)—The largest lobbying group for health insurers has asked U.S. lawmakers weighing the fate of Obamacare to push back the due date for 2018 individual insurance submissions to regulators in hopes of obtaining greater clarity on the program’s future later on. Republican leaders including President-elect Donald Trump and U.S. Senate Majority Leader Mitch…
New York City Hospitals Settle Medicaid Repayment after Fraud Charges
NEW YORK (Reuters)—Three hospitals in New York’s Mount Sinai Health System will pay $2.95 million to settle Medicaid fraud charges for taking two years to repay more than $844,000 of improper billings that had been flagged by a whistleblower, authorities say on Wednesday. The accord resolves claims that Mount Sinai Beth Israel, Mount Sinai St….

2016 ACR/ARHP Pre-Meeting Educational Workshops to Cover MACRA, Merit-Based Incentive and Alternative Payment Models
Looking for a reason to attend the 2016 ACR/ARHP Annual Meeting, which will be held Nov. 11–16 in Washington, D.C.? This monumental meeting will offer a variety of sessions on MACRA/MIPS/APMs, Medicare Value-Based Payment Reform programs, auditing, compliance and coding. Particularly, the pre-meeting workshops will provide you with the unique opportunity to dive deep into…
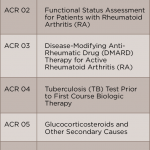
Rheumatology Informatics System for Effectiveness (RISE) Registry Can Help Rheumatologists Meet MACRA Requirements
The ACR has been at the forefront of helping rheumatologists meet practice demands, including federal reporting requirements. The first registry that helped meet these requirements was the Rheumatology Clinical Registry (RCR), and it facilitated quality reporting, but required manual entry of required data. More recently, ACR has contracted with FIGmd to create a tool that…
Health Has Improved in States That Expanded Low-Income Insurance Options
(Reuters Health)—In states that expanded either their Medicaid programs or private insurance options for low-income Americans, beneficiaries used more outpatient and preventive care and less emergency care. They also had better subjective overall health, compared with low-income residents of states with no expanded coverage. All states participate in Medicaid, a partnership with the federal government…

Avoid the Trap of Balance Billing
It is no secret that payers and providers have conflict as it relates to reimbursement rates for medical services, and there is another stakeholder, the patient, that plays an important role in the financial impact of healthcare reimbursement. Usually, patients are faced with unforeseen bills from their providers due to an unpaid portion of a…
Anthem CEO Backs Obamacare Insurance Exchanges & Sees Possible Growth
(Reuters)—Health insurer Anthem Inc. on Wednesday said the Obamacare individual insurance exchanges are not as profitable as it originally expected, but it is not planning to exit like competitor UnitedHealth Group. Anthem Chief Executive Officer Joseph Swedish said the company had picked up more exchange customers than it expected during the first quarter and that…

What Rheumatologists Need to Know about Payer Audits
Both government and private payers continue to aggressively monitor providers to prevent and recover overpayments. This is evidenced by the fact that the number of audits conducted in recent years has increased dramatically. A negative audit finding can result in the need to repay five- or seven-figure amounts. Types of Audits Private Payer Audits Private…
U.S. Proposes Hike in Medicare Advantage Payments; Insurer Shares Rise
NEW YORK (Reuters)—The U.S. government on Friday proposed raising payments by 1.35% on average next year to the health insurers who offer Medicare Advantage health benefits to elderly and disabled Americans. Payments to insurers will vary under the 2017 Medicare Advantage proposal, based on the region the plans are sold and on the size of…
Pfizer Unit to Pay $784.6 Million in Medicaid Rebate Settlement
(Reuters)—Pfizer Inc. said its Wyeth unit has agreed to pay $784.6 million to settle cases related to the calculation of Medicaid rebates for a gastric drug between 2001 and 2006. The claims alleged that Wyeth’s calculation of rebates for its proton pump inhibitor Protonix (pantoprazole) violated the Federal Civil False Claims Act and other laws…