The latest research on imaging & treatment for GCA presented at ACR Convergence 2025
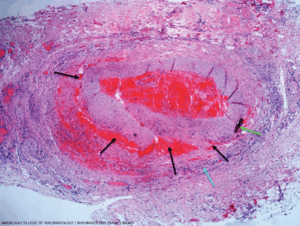
This temporal artery biopsy from a 73-year-old man with jaw claudication and acute vision loss shows vessel wall inflammatory infiltrates (blue arrow) with rare giant cells and loss of the internal elastic lamina. (Click to enlarge.)
CHICAGO—Giant cell arteritis (GCA) is the most common form of systemic vasculitis in older adults, but until recently, we had relatively little to offer patients with this diagnosis. Recent years have seen an explosion of research, leading to substantial advances in the assessment and treatment of GCA. Here, we highlight some of the most exciting GCA-related research presented at ACR Convergence 2025.
1. Efficacy & Safety of Upadacitinib
Schmidt et al., Abstract 07761
In April, the U.S. Food & Drug Administration (FDA) approved upadacitinib, an oral Janus kinase (JAK) inhibitor, for the treatment of GCA based on SELECT-GCA, a double-blind, randomized trial. This study demonstrated that 15 mg of upadacitinib taken daily combined with a 26-week glucocorticoid taper was superior to treatment with a 52-week glucocorticoid taper at achieving sustained remission in patients with GCA.2
In a follow-up study presented by Schmidt et al., patients who remained on upadacitinib for an additional year had a higher sustained remission rate than patients who stopped therapy (68.6% vs. 28.6%), leading to a 90% reduction in the risk of disease flare from week 52 to week 104. Patients who remained on upadacitinib continuously for two years also required less glucocorticoids to remain in remission than patients who stopped therapy after one year. Additionally, patients treated with 15 mg of upadacitinib daily over two years had higher rates of herpes zoster and elevated creatine kinase, but lower rates of serious infection, and no increased risk of venous thromboembolism, major adverse cardiovascular events or death.1
Many clinicians have been reluctant to consider prescribing JAK inhibitors for older patients, given that the ORAL Surveillance clinical trial demonstrated a potential association between tofacitinib and several adverse events, including venous thromboembolism and major adverse cardiovascular events.3 However, the current study with two-year follow-up data from the SELECT-GCA trial implies that long-term therapy with upadacitinib is well tolerated. This finding is fortunate because the results also indicate that many patients may benefit from prolonged drug therapy.
2. Glucocorticoid Tapering
Buttgereit et al., Abstract 08954
In another analysis of the SELECT-GCA study, investigators focused on the effect of upadacitinib on serious infections, herpes zoster and opportunistic infections.


