DESTIN, FLORIDA—During the Congress of Clinical Rheumatology (CCR) East meeting in May, Michelle Petri, MD, MPH, MACR, professor of medicine in the Division of Rheumatology and director of the Johns Hopkins Lupus Center, Johns Hopkins School of Medicine, Baltimore, presented a talk titled 10 Things I Want You to Know about Lupus.
DESTIN, FLORIDA—During the Congress of Clinical Rheumatology (CCR) East meeting in May, Michelle Petri, MD, MPH, MACR, professor of medicine in the Division of Rheumatology and director of the Johns Hopkins Lupus Center, Johns Hopkins School of Medicine, Baltimore, presented a talk titled 10 Things I Want You to Know about Lupus.
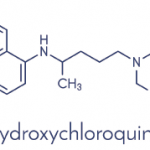
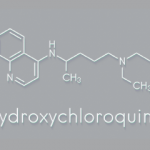
HCQ Use in SLE
The first pearl Dr. Petri offered is the benefit of hydroxychloroquine (HCQ) and how it should be used as a background therapy for all patients with systemic lupus erythematosus (SLE). She explained HCQ should not be tapered in a patient with quiescent lupus because multiple studies have demonstrated an improvement in survival and reduction in organ damage and cardiovascular risk in those taking the drug. She explained her disagreement with the ophthalmology and ACR weight-based guidelines for HCQ, although she agrees with the need for retinal toxicity monitoring.
“What I don’t want anybody to do … is [follow] the 5 mg/kg rule because that means you will be underdosing a lot of patients,” Dr. Petri said. “If the whole blood [HCQ] level is subtherapeutic, the patient is not getting a benefit from it.”
Dr. Petri instead recommends obtaining a whole blood HCQ level to fine tune the optimal dosage.
Next, Dr. Petri discussed a second pearl on HCQ retinopathy. The risk of retinopathy is low in the first 10 years of use. Central serous retinopathy is an important mimic of HCQ retinopathy seen in patients taking high doses of glucocorticoids. She emphasized the importance of direct communication with ophthalmology when there is confusion regarding the etiology of an abnormal eye exam or inappropriate recommendations.
HCQ whole blood levels can also be used to stratify patients for retinopathy risk.
“If a patient has whole blood hydroxychloroquine levels above 1,200 ng/mL consistently, visit after visit, that patient has an increased risk [of HCQ retinopathy],” Dr. Petri said. She recommended maintaining HCQ whole blood levels “in the optimal range, 750–1,200 [ng/mL].”
Vitamin D in Lupus Pregnancy
Dr. Petri’s third pearl urged rheumatologists to understand the role of vitamin D in SLE. “We found up to a 25-hydroxy vitamin D level of 40 significantly reduces urine protein,” she said.
Maternal fetal medicine experts are also recommending vitamin D supplementation in pregnancy in the general population because data suggest it reduces adverse pregnancy outcomes, according to Dr. Petri. She studied vitamin D levels in pregnant patients with SLE, but found a U-shaped association between vitamin D level and adverse pregnancy outcomes.1