“All patients should be treated to get their disease to at least a low level of disease activity (even better, to remission),” he said. He emphasized that rheumatologists need to be more aggressive in their use of methotrexate (MTX) in this stepped-up approach to disease management with the conventional disease-modifying antirheumatic drugs (DMARDs).
He urges rheumatologists to start with aggressive treatment with MTX that may include pushing the dose up to 25 mg per week subcutaneously. “This will control 28% to 45% of patients,” he said. In patients in whom this is an insufficient target to control active disease, he advises using triple therapy. “This will control 25% more of patients,” he said. If this treatment still doesn’t reach the target, he then would move on to the use of biologics.
He emphasized, however, that before patients move on to expensive biologics they should use triple therapy.
To support this treat-to-target approach, he cited evidence from five investigator-initiated trials over the past 10 years that he said show that conventional DMARD therapy should be the first option in the initial treatment of RA and in patients with active disease despite treatment with MTX (see Table 1).
He said that the TEAR, BeSt, and TICORA trials all clearly show that patients with new-onset RA treated to target with strategies that start with DMARD combinations have comparable clinical outcomes to patients started on biologics. He also highlighted the most recent findings from the RACAT trial that showed for the first time that triple therapy is noninferior to etanercept clinically and radiographically in patients with RA who have active disease despite MTX treatment.
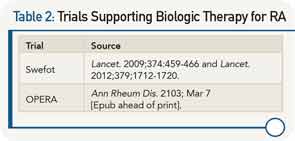
In discussing the Swefot trial, he pointed out that this was not a treat-to-target trial and emphasized that the data from the trial showed no clinical differences at six, nine, or 24 months between patients with early RA who fail MTX treated with the addition of infliximab or those treated with conventional DMARDs.
Underlying the focus on the treat-to-target approach was the emphasis on trying the lower-cost DMARDs before moving on to the much costlier biologics. He used the analogy of a three-legged stool to emphasize the three main issues that need to be considered to support choosing one therapy over another. Along with efficacy and toxicity, cost is equally important to consider. “No healthcare system in the world can afford to have more than 50% of patients with RA on biological therapy,” he said, adding that, fortunately, with the data now available, quality care can be provided much less expensively.