1) Obesity & Treatment Response in RA
Obesity & response to advanced therapies in rheumatoid arthritis
Why was this study done? There have been questions regarding whether certain therapies for rheumatoid arthritis (RA) are less effective in patients with obesity, particularly for tumor necrosis factor (TNF) inhibitors, because adipose tissue is known to generate TNF, among other inflammatory mediators.
What were the study methods? We studied 5,901 patients enrolled in the CorEvitas registry who were initiating a TNF inhibitor or a non-TNF inhibitor biologic. We used linear and logistic regression to look at response to therapy across a range of body mass indexes (BMI). We first looked at response to any therapy, then tested to see whether any observed effect of obesity on response differed between those initiating a TNF inhibitor and those initiating a non-TNF biologic. We adjusted analyses for potential confounding factors, such as age, disease activity and comorbidities.
What were the key findings? There were three main observations. First, obesity was associated with a reduced response to therapy, although the effect was modest after adjustment. Specifically, patients with obesity had modestly lower odds of achieving low disease activity six months after starting a biologic therapy (odds ratio [OR]=0.88).
Second, there was no difference in this effect whether the person received a TNF inhibitor therapy or a non-TNF inhibitor therapy, suggesting the lack of response in this group was not treatment specific.
Third, underweight patients were much less likely to respond to both types of therapies (OR=0.32) even after adjustment. With regard to these observations, it didn’t seem to matter whether the medication used weight-based dosing.
What were the main conclusions? Although obese and underweight patients may indeed show lower responses to therapy, this is not therapy specific.
What are the implications for patients? When starting therapy, underweight and obese patients should recognize the treatment may not be as effective for them as for others—although it’s not clear the treatment strategy should be different.
What are the implications for clinicians? The impact of obesity on health is broad, which may explain why lower clinical responses are observed for multiple types of therapies with different mechanisms of action. Obesity may cause persistent symptoms of obesity-related conditions (e.g., osteoarthritis, fibromyalgia) and promote systemic inflammation through release of cytokines and adipocytokines. Underweight patients may have experienced cachexia due to a high burden of systemic inflammation; this may explain the lower responses observed in this group.
The Study: Baker JF, Reed G, Poudel DR, Harrold LR, Kremer JM. Obesity and response to advanced therapies in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2022 Feb 10. doi: 10.1002/acr.24867. Epub ahead of print. PMID: 35143117.
2) Risk Factors for CPPD
Proton pump inhibitors & the risk of calcium pyrophosphate deposition in a population-based study
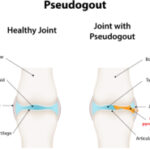
Why was this study done? Calcium pyrophosphate deposition disease (CPPD) is common among older adults, but no therapies specifically target CPPD. Hypomagnesemia is associated with the risk of CPPD, and proton pump inhibitor (PPI) use is associated with hypomagnesemia. This study investigated whether PPI use is a risk factor for incident CPPD.
What were the study methods? We used data from the U.K.-based IQVIA Medical Research Database. First, we conducted a propensity score-matched cohort study to compare the risk of incident CPPD among PPI users vs. histamine receptor 2 (H2) blocker users. We used multivariable Cox proportional hazard models, censoring subjects at the time of drug switch. In our second study design, we evaluated incident use of PPI and H2 blockers prior to incident CPPD, using a nested, case-control study, matched 1:4 by age and sex.
What were the key findings? We did not find evidence that incident PPI use was associated with a higher risk of CPPD when compared with H2 blocker use. In the casecontrol study, when compared with non-users, both PPI and H2 blocker users had a higher risk of incident CPPD. Incident PPI use was not significantly associated with incident CPPD, compared with H2 blocker use.
What are the main conclusions? Incident use of PPIs was not significantly associated with an increased risk of CPPD compared with incident H2 blocker use in either study design. However, due to few CPPD cases, we had limited precision in detecting small treatment effects, so this does not rule out a causal association. The results from the case-control study are interesting: It is possible that H2 blocker use may have a similar effect to that of PPI use because users of both medications had a higher risk of CPPD than people who did not use either medication. Confounding by indication cannot be ruled out in this observational study.
What are the implications for patients? Patients diagnosed with CPPD should be ready to review their medication lists with their providers. Patients who are on PPIs in the long term should discuss the need for continuing this therapy.
What are the implications for clinicians? It may be reasonable to re-evaluate the need for long-term PPIs among patients with difficult-to-manage CPPD.
The Study: Liew JW, Peloquin C, Tedeschi SK, et al. Proton pump inhibitors and risk of calcium pyrophosphate deposition in a population-based study. Arthritis Care Res (Hoboken). 2022 Mar 4. doi: 10.1002/acr.24876. Online ahead of print.
3) Disparities Persist
Race, ethnicity & disparities in the risk of end-organ lupus manifestations following SLE diagnosis
Why was this study done? Prior research has shown that many racial and ethnic groups in developed countries experience a disproportionate burden of systemic lupus erythematosus (SLE). We know less about the time course of severe SLE across organ domains by race and ethnicity.
What were the study methods? Adults with SLE in the California Lupus Epidemiology Study participated in annual study visits in which data on lupus manifestations were collected by a lupus expert. Self-reported race and ethnicity were categorized as non-Hispanic white, Hispanic, non-Hispanic Black and non-Hispanic Asian. Major end-organ lupus manifestations were categorized into the following organ systems: renal, hematologic, neurologic, cardiovascular, and pulmonary disease. Multi-organ disease was defined as manifestations in two or more of these distinct organ systems. Survival analysis methods were used to analyze the risk of end-organ manifestations following SLE diagnosis for Hispanic, Black and Asian participants compared with white participants, adjusting for sex and age at diagnosis.
What were the key findings? The racial and ethnic distribution of the cohort was 30% white, 23% Hispanic, 11% Black and 36% Asian. Renal and hematologic disease occurred early during the SLE disease course. Multi-organ disease was present in 29% of individuals with SLE; renal disease was concurrent in most cases of multi-organ disease. Hispanic and Asian participants with SLE had two- to threefold higher risks of renal, hematologic and multiorgan disease following diagnosis than white participants, adjusting for sex and age at diagnosis.
What are the main conclusions? In this study conducted in the U.S., we show that Hispanic and Asian individuals with SLE are at higher risk for developing renal, hematologic, and multiorgan manifestations of SLE than white individuals; in addition, Hispanic and Asian individuals develop these manifestations faster than white individuals. More than a quarter of participants had multi-organ involvement from SLE.
What are the implications for patients? People with SLE are encouraged to discuss their risk of lupus manifestations with their clinicians, and interventions that can ameliorate this risk.
What are the implications for clinicians? Our study highlights that people with early SLE should be closely monitored for development of new or additional severe lupus manifestations, and that special vigilance is required in Hispanic and Asian patients.
The Study: Aguirre A, Izadi Z, Trupin L, et al. Race, ethnicity, and disparities in risk of end-organ lupus manifestations following SLE diagnosis in a multiethnic cohort. Arthritis Care Res (Hoboken). 2022 Apr 22. doi: 10.1002/acr.24892. Online ahead of print.