Even after the diagnosis of IIM has been established, MRI remains useful to monitor response to treatment, qualitatively measure disease activity, and direct future management. This is particularly important when discordance exists between the patients’ symptoms and providers’ assessments and when routine serologic markers of muscle breakdown fail to correlate with clinical findings. Active disease requiring escalation or modification of therapy is indicated by more pronounced muscle edema, whereas response to therapy appears as resolution or reduction of edema (normalization of intensity values or “return to isointensity” in the above sequences). Notably, a relationship between the degree of STIR hyperintensity and the abundance of pre-treatment inflammatory infiltrates on muscle biopsy has been shown in several studies.4,6
On the other hand, intensification of the largely irreversible markers of chronicity and damage, such as fatty replacement and atrophy (increased signal intensity and decreased muscle mass, respectively, on T1W), warrant reevaluation of the drug regimen to balance out the need to prevent both disease progression and unnecessary exposure to potentially harmful medications. Quantitative MRI studies have similarly demonstrated a modest correlation between the extent of fatty infiltration noted on MRI and that seen on muscle histopathology.7,8
Thus, the capacity of MRI findings to correlate with response to therapy underscores its value in guiding subsequent decision making. With its versatility, granularity and increasing ubiquity, it’s easy to see why MRI is the go-to muscle imaging modality (see Table 2).
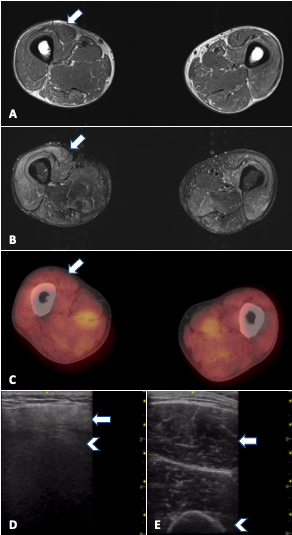
FIGURE 1. MRI, PET/CT and ultrasound in a 33-year-old man with refractory PM-Scl dermatomyositis. Arrows: rectus femoris; arrowheads: humerus. A) MRI of the thighs (T1W) showing no significant fatty replacement. B) MRI of thighs (STIR) with mild to moderate muscle edema (increased signal) mainly in anterior compartment. C) PET/CT showing symmetric bilateral increased FDG uptake in scattered muscles, especially pelvic adductors, D) increased muscle echointensity in the rectus femoris with attenuation (loss of bone echo of underlying femur) and atrophy in comparison with E) normal rectus femoris in age-matched control.
Ultrasound
Ultrasound is undeniable proof that oldies can still be goodies. With the advent of higher frequency probes, imaging resolution for soft tissue is now far higher than MRI and offers a close-up view of the muscle, which has its own advantages. Ultrasound also has more widespread availability, portability, cost efficiency, and real-time imaging capability, with the latter rendering it a useful tool for optimizing muscle biopsy site selection as well as for detecting abnormal muscle movements (see Table 2). However, ultrasound is heavily operator dependent, and knowledge of both proper image acquisition and image interpretation for muscle is needed.


