It is important to note that not all instances of MRI-detected muscle edema in IIM correlate with an increase in 18F-FDG activity. The detection of increased 18F-FDG activity may provide another layer of information regarding the disease process (see Figure 1C, right). Additionally, its utility in screening for malignancy in newly diagnosed or refractory cases of myositis is being invoked, as well as its ability to follow interstitial lung disease.18,19
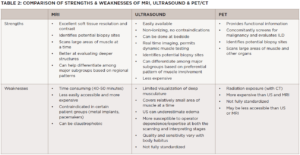
PET imaging may be uniquely advantageous to the subset of patients considered at high risk for malignancy and interstitial lung disease based on autoantibody status and other predictors (see Table 2). PET/MR, which offers higher soft tissue contrast than PET/CT without the ionizing radiation, may yet emerge as a mainstream modality in IIM imaging.
Conclusion
A thorough clinical evaluation aided by serologic and histopathologic findings remain at the forefront of the assessment and management of IIMs; however, there is plenty of room to harness the power of imaging studies, such MRI, ultrasound and multimodal PET to better characterize disease parameters across the entire clinical trajectory. While each modality can certainly hold its own in the myositis imaging space, they can also be used either simultaneously or sequentially to paint the most accurate picture of a patient’s condition over time.
Capitalizing on the major strengths of each imaging approach—the clarity for muscle edema vs. fat/fibrosis with MRI, the real-time and dynamic assessment with ultrasound, and the physiologic information of PET—can provide clinicians with the images that best capture what is needed to positively influence decision making and overall outcomes.
With the broad shift toward less invasive, more patient-centric approaches in all aspects of patient care, these pictures will certainly be worth far more than a thousand words in the not-too-distant future.
 Rochelle L. Castillo, MD, MS, is a clinical instructor in the Division of Rheumatology at NYU Grossman School of Medicine, New York, where she also completed her rheumatology fellowship. She is a clinician-investigator with a specific interest in conditions that bridge the rheumatology-dermatology interface, such as psoriatic disease and dermatomyositis.
Rochelle L. Castillo, MD, MS, is a clinical instructor in the Division of Rheumatology at NYU Grossman School of Medicine, New York, where she also completed her rheumatology fellowship. She is a clinician-investigator with a specific interest in conditions that bridge the rheumatology-dermatology interface, such as psoriatic disease and dermatomyositis.
 Andro Licaros, MD, is a clinical fellow in the Cancer Imaging Program at Dana-Farber Cancer Institute/Harvard Cancer Center, Boston. His research work focuses on cancer imaging, and quality and safety improvements in radiology leveraging machine learning and artificial intelligence toward patient-centric outcomes.
Andro Licaros, MD, is a clinical fellow in the Cancer Imaging Program at Dana-Farber Cancer Institute/Harvard Cancer Center, Boston. His research work focuses on cancer imaging, and quality and safety improvements in radiology leveraging machine learning and artificial intelligence toward patient-centric outcomes.
 Jemima Albayda, MD, is an assistant professor of medicine in the Division of Rheumatology at the Johns Hopkins University School of Medicine, Baltimore. She is the director of the Rheumatology Fellowship Program, as well as the Musculoskeletal Ultrasound and Injection Clinic. Her clinical and research focus is in the inflammatory muscle diseases, musculoskeletal ultrasound and arthritis.
Jemima Albayda, MD, is an assistant professor of medicine in the Division of Rheumatology at the Johns Hopkins University School of Medicine, Baltimore. She is the director of the Rheumatology Fellowship Program, as well as the Musculoskeletal Ultrasound and Injection Clinic. Her clinical and research focus is in the inflammatory muscle diseases, musculoskeletal ultrasound and arthritis.
References
- Lundberg IE, Tjärnlund A, Bottai M, et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann Rheum Dis. 2017 Dec;76(12):1955–1964.
- Costa AF, Di Primio GA, Schweitzer ME. Magnetic resonance imaging of muscle disease: A pattern-based approach. Muscle Nerve. 2012 Oct;46(4):465–481.
- Tomasová Studýnková J, Charvát F, Jarošová K, Vencovský J. The role of MRI in the assessment of polymyositis and dermatomyositis. Rheumatology (Oxford). 2007