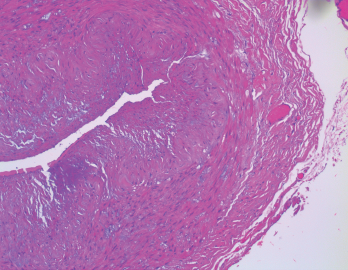
Figure 1. The biopsy of the right temporal artery with hematoxylin and eosin (H&E) staining was unremarkable.
Sarah2 / shutterstock.com
Giant cell arteritis (GCA) is a granulomatous vasculitis of large- and medium-sized arteries, usually affecting the cranial branches of the aortic arch. It is the most common vasculitis, with the highest risk factor being age. Accurate diagnosis and prompt initiation of therapy are of great importance to prevent serious complications, with the most feared being permanent vision loss.
The diagnosis is suspected clinically based on characteristic symptoms and laboratory findings, and confirmed histologically by temporal artery biopsy.
A classical presentation is easy to recognize when a patient older than 50 presents with a new-onset headache along with other characteristic findings, such as jaw claudication, symptoms of polymyalgia rheumatica (PMR) and elevated inflammatory markers. In clinical practice, however, GCA often presents diagnostic and management challenges.
These challenges arise from different factors, including:
- An atypical presentation (e.g., no headaches or atypical headaches, normal inflammatory markers or rare presenting symptoms, such as tongue or limb claudication, chronic cough, vertigo or oculomotor nerve palsy);
- A negative temporal artery biopsy despite the high probability of the disease based on clinical presentation. In this case, the clinician has to make the difficult decision to continue high-dose steroid therapy, which comes with the potential of serious adverse effects, or to stop therapy and risk serious complications, such as permanent vision loss;
- Temporal arteritis due to another form of systemic vasculitis, such as anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis or polyarteritis nodosa (PAN); or
- Intolerance to high-dose steroid therapy.
We present a case that highlights some of these challenges and provide some clinical pearls that can help in the diagnosis and management of GCA.
Case Presentation
Our patient is a 78-year-old woman with a past medical history of hypertension and osteoporosis. She initially presented to the emergency department with new-onset neck pain and headache that started after a long bus ride one week earlier.
The pain started as a right-sided posterior neck pain, which radiated to the right occipital scalp and then anteriorly toward the right frontal area. She described the pain as intermittent, sharp, shooting and severe, at times.
She had no constitutional symptoms, jaw claudication or proximal myalgias. Her neurological examination was normal. Magnetic resonance imaging (MRI) of the brain was obtained because of her acute-onset, severe headache, but was unremarkable. MRI of the cervical spine showed age-related degenerative changes.
Her laboratory evaluation was significant for a markedly elevated erythrocyte sedimentation rate (ESR) of 73 mm/hr (reference range [RR]: 0–15 mm/hr) and C-reactive protein (CRP) of 87 mg/L (RR: <5–10 mg/L).
She underwent a unilateral right temporal artery biopsy (see Figures 1&2, above and opposite) and was started on 60 mg of prednisone daily for suspected GCA. Her headaches mildly improved, but her temporal artery biopsy result was did not demonstrate evidence of vasculitis. Given her negative biopsy results, GCA was considered unlikely, and the prednisone was tapered off over two weeks.

