I had a patient at the Veteran’s Administration (VA) hospital whom I frequently treated during the last two months of my rotation at that facility. While I need not share the specific details of his illness, the patient is perhaps the most important component of this musculoskeletal ultrasound (MSUS) story.
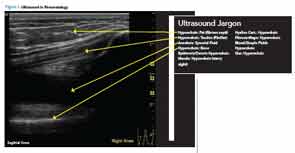
My experience with ultrasound (US) did not begin at the VA. I generally was familiar with this technique before starting my fellowship. Using US as the joints’ imaging modality emerged in American rheumatology over a decade ago. MSUS uses the concept of tissue echogenicity, which refers to the ability to reflect or transmit US waves against the surrounding tissues. The difference in tissue context—echogenicity—is visible on the US monitor as a change in contrast. Based on echogenicity, commonly referred to as gray scale, a structure can be defined as hyperechoic, seen as white on the screen, hypoechoic gray and anechoic black (see Figure 1, opposite). MSUS can augment recognition of active inflammation with the use of color Doppler where increased signal identifies better perfused, diseased tissue.
When I became aware that the VA had a US machine available for rheumatology use, I became interested in gaining some experience with the technique during my rotation there. My patient proved not only an enthusiastic model for scanning, but also an agent provocateur, stimulating my interest in polishing my skills with this technique.
Key to Abbreviations
- ACR’s RhMSUS: The American College of Rheumatology’s Musculoskeletal Ultrasound Certification in Rheumatology
- MSUS: musculoskeletal ultrasound
- PAN: polyarteritis nodosa
- UCLA: University of California in Los Angeles
- UTSW: Texas Southwestern University
- VA or VAMC: Veterans Affairs Medical Center
Patient Response to US Years ago my patient was diagnosed with polyarteritis nodosa (PAN) that doesn’t follow any pattern or respond to any treatment. His situation was one of those for which no trial helped guide me toward a choice of therapy, no expert opinion moved me forward, no state-of-the-art lecture provided me with an “aha moment.” His illness kept me awake at night.
Ultrasound machines are expensive. Their luxury-car price tag explains why the one at the VA was garaged in the office of the chief of rheumatology, located on the fifth floor. Three mornings a week, I wrestled with the machine, transporting it down four floors to the exam room, in and out of elevators, zig-zagging between the waiting room seats, trying to avoid inflicting damage to any federal property. One day, my patient saw me rolling this cumbersome machine into the exam room and commented on “what a nice toy” it seemed to be. I explained how the US beam allowed me to see small fragments of tissue. His interest piqued, my patient immediately volunteered to be scanned. As a veteran and a beneficiary of the VA medical system, he saw himself as part owner of the machine and felt obliged to help me maneuver the machine.
My patient gladly let me scan his hands to see whether he had responded to treatment (sadly, he rarely did). He was fascinated whenever I froze those confusing black, grey and white lines and shadows on the screen. I tried to explain what each of these meant. Rather quickly, I realized that negative scans may be as important as those grossly positive, allowing me to redirect the focus of my care and move forward. My patient encouraged me to pursue this technique and provided me the opportunity to figure out for myself the logistics of whether and how to use MSUS, and how to interact with the patient and staff during the MSUS visit. I moved out of the knowledge-acquisition twilight zone and into the realm of the advanced learner.
My patient’s keen approach toward the US was not an isolated response. Many of my VA patients thought MSUS was cool. Although I usually had just enough time to perform focused joint exams, patients often requested that I scan additional joints during the future visits. At their request, and when appropriate, I visualized fluid pockets in knees, placed the needle and the steroids in the exact joint spaces, and analyzed the presence or absence of the tissue inflammation.
I think that such positive feedback is an important aspect of patient-centered medicine. Indeed, some have argued that patient satisfaction is often indicative of the quality of patient care.1 (Editor’s note: See Speak Out Rheumatology)
Challenges to Using US in Rheumatology
It has been observed that rheumatology fellows and those in practice for less than five years are those caregivers most interested in learning MSUS technique.2 But my mentor, David Minna, MD, of Dallas, is a stark exception to this rule. He didn’t get interested in MSUS until about 25 years into his career. He liked performing procedures and was intrigued by the early challenges of US: the technical aspect of its use, learning how to incorporate US into a busy practice and determining how best to finance this new but expensive professional tool. Finding teachers on how to use and apply ultrasound in rheumatology was a challenge, and a considerable part of his learning curve was based on self study.
Based on a 2010 fellowship program directors survey, less than half of the programs had a faculty member who was performing US in their practices.3 Perhaps the greatest challenge to expanding MSUS in rheumatologic care, besides lack of education and equipment cost/availability issues, is convincing colleagues to break the habit of referring many of their patients to radiology for more costly imaging. How will we succeed? Changing medical culture is never easy, but rheumatology fellows should have access to MSUS during their training. Not only can it help establish specific diagnoses, the technique also requires the student to know the relevant musculoskeletal anatomy. This knowledge can only help us in the management of our patients with rheumatologic diseases.
I suggest that, in patient-oriented medicine, patients’ perceptions of MSUS results may promote its expanded use. The images are confusing at first, but with minimal on-the-spot education, the scans can help patients visualize and understand key clinical concepts of their disease process, such as abnormal joint effusion or enlargement (see Figure 2).
Some rheumatologists are critical of ultrasound’s use and doubt the tool will gain broader future acceptance. There are indeed valid concerns with regard to insurer payment, lack of support for training and inter-reader scanning reliability.2
The appropriateness of allocating time for US scanning during fellowship training has been questioned. Arguably, the additional minutes could be put to more beneficial use developing more detailed chart review, better joint examination or other visit-related, patient-oriented activities. Presently, the best response to these concerns is unknown, and only time will tell how rheumatologists adapt to the new practice environment.
Why Ultrasound Is Important
On the other hand, researchers have accumulated evidence of improved detection of synovitis using US while assessing inflamed joints of patient with rheumatoid arthritis and ensuring greater precision when injecting selected joints.4,5
My own experience with ultrasound has allowed me to detect synovial fluid with certainty, better direct the injection needle, accurately diagnose shoulder pathology on the spot and immediately share what I saw with the patient.
MSUS is a great tool for both the practitioner and the patient. It has a great future in our specialty.
Katarzyna Gilek-Seibert, MD, is a second-year rheumatology fellow at UTSW Medical Center in Dallas.
References
- Nelson EC, Larson CO, Davies AR, et al. The patient comment card: A system to gather customer feedback. QRB Qual Rev Bull. 1991;Sep;17(9):278–286.
- Samules J, Abramson SB, Kealey GS. The use of musculoskeletal ultrasound by rheumatologists in the United States. Bull NYU Hosp Jt Dis. 2010;68(4):292–298.
- Whorton Marketing and Research. 2010 musculoskeletal ultrasound research: Training directors survey (Nov. 23–Dec. 10, 2010). Survey: American College of Rheumatology MSUS Certification Task Force; 2010.
- Szkudlarek M. Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Arthritis Rheum. 2003 Apr;48(4):955–962.
- Lawson A, Kelsberg G, Safranek S. Clinical inquiry: Does ultrasound guidance improve outcomes for steroid joint injections? J Fam Pract. 2013 Dec;62(12):763a–763c.