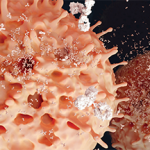
NEW YORK (Reuters Health)—Patients with untreated early rheumatoid arthritis (RA) show signs of immune activation and local inflammation in their bronchial tissues, researchers from Sweden report.
Previous studies have shown that patients with RA have shared citrullinated epitopes in the lungs and joints, as well as anticitrullinated protein antibodies (ACPA) in bronchoalveolar lavage (BAL), suggesting that RA-associated autoimmunity could begin in the lung compartment.
Dr. Anca I. Catrina and colleagues from Karolinska Institute, Stockholm, sought to characterize lymphocytic infiltration in the large and small airways of 24 patients with early, untreated RA without clinical lung disease as part of the LUng investigations in early RA (LURA) study.
ACPA-positive patients had evidence of airflow limitations and decreased gas transfer, compared with ACPA-negative patients. ACPA-positive patients were also more likely than other RA patients to have evidence on high-resolution computed tomography (CT) of parenchymal and airway changes.
Bronchial biopsies showed frequent lymphocytic infiltration, along with expression of immune activation markers, especially in ACPA-positive patients, according to the Nov. 3 Annals of the Rheumatic Diseases online report.
Compared with controls, ACPA-positive (but not ACPA-negative) patients had increased numbers of B and T lymphocytes and reduced numbers of macrophages in BAL fluid.
“The possibility that early changes (such as the ones described here) might also to a certain extent be due to a direct antibody-mediated injury and/or low-grade inflammation already before disease onset cannot be completely excluded,” the researchers note. “Isolation of ACPA-producing B cells from the lung compartment would be the final proof of local immune activation and antibody production, and this still remains to be done.”
“In conclusion, we have demonstrated signs of immune activation in BAL and bronchial biopsies of patients with early untreated ACPA-positive RA,” they write. “This strengthens the hypothesis that the lung plays an important role in the immunological reactions responsible for the development of ACPA-positive RA, and warrants further functional and interventional studies to address this pathogenic link.”
Dr. Catrina did not respond to a request for comment.
This research had multiple supporters. The authors reported no disclosures.