Even with prompt recognition, acute hemorrhagic myositis can cause abrupt hemodynamic collapse & rapid progression to death.
His primary care physician consulted a hepatologist, due to concern for autoimmune hepatitis, and initiated empiric doxycycline with concern for tick-borne illness.
A recheck of laboratory studies during the current presentation revealed AST 191 U/L (normal: 15–41 U/L), ALT 76 U/L (normal: 17–63 U/L), ALP 112 U/L (normal: 24–110 U/L), albumin 1.8 g/dL (normal: 3.5–4.8 g/dL), aldolase 17.8 U/L (normal: <7.7 U/L), and peak creatine kinase (CK) 2,848 U/L (normal: 30–220 U/L). Creatinine and complete blood count tests were within normal limits. His CRP (2.79 mg/dL) and ferritin (735 ng/mL) were elevated, but his erythrocyte sedimentation rate was within the normal range.
Positive serologies included ANA 1:2560 with cytoplasmic speckling, AMA 39.9 U, RF 88 IU/mL, and anti-ribonuclear protein (RNP) 193 AU/mL. The MyoMarker Panel 3 was notable for an elevated anti-transcription intermediary factor 1-γ (TIF1-γ) at 126 U (normal: <20 U).
A contrast computerized tomography (CT) scan of his chest, abdomen and pelvis revealed numerous enlarged and heterogeneously enhancing mediastinal and right hilar lymph nodes (see Figure 2).

Figure 2. A contrasted CT scan of the chest shows numerous pathologic mediastinal and right hilar lymph nodes (maroon arrow).
Magnetic resonance imaging scan with myositis protocol of his lower extremities showed extensive symmetric T2 hyperintense signal involving the bilateral thigh and pelvis musculature with evidence of subcutaneous and perifascial edema consistent with myositis (see Figure 3).
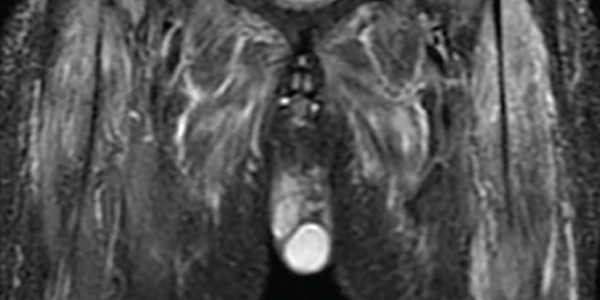
Figure 3. An MRI myositis protocol of the lower extremities with extensive, symmetric edema-like T2 signal of both thighs and the pelvis musculature.
Electromyography revealed abundant spontaneous activity in the form of fibrillation potentials and positive sharp waves in the deltoid and biceps brachii; it showed myopathic motor unit action potentials with early recruitment, consistent with an inflammatory myopathy.
A videofluoroscopic swallow study showed no oropharyngeal dysphagia. He underwent endobronchial ultrasound-guided fine needle aspiration biopsy of multiple lymph nodes. Rare tumor cells were present, with immunohistochemical testing positive for cytokeratin 7, suggestive of adenocarcinoma, and weakly positive for thyroid transcription factor 1, suggestive of a lung primary adenocarcinoma (see Figure 4).
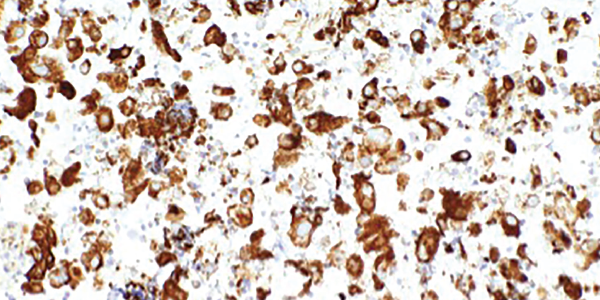
Figure 4. An ultrasound-guided, fine-needle aspiration biopsy of the mediastinal lymph nodes shows rare tumor cells. Immunohistochemical testing revealed the presence of cytokeratin 7 and thyroid transcription factor 1.
Next-generation sequencing was remarkable for missense mutations of NRAS, which are more commonly found in adenocarcinomas with a history of tobacco use, and TP53, which can be seen in a number of malignancies including lung cancers.2,3
Left forehead and right eyebrow lesion shave biopsies showed nodular and infiltrative pattern basal cell carcinoma, respectively. A right deltoid muscle biopsy demonstrated myopathic changes, fiber necrosis, fiber atrophy and minimal inflammatory cells, with no evidence of hemorrhage, granulomas or vasculitis (see Figure 5).


