The classic description of symptoms includes arthritis, fever, evanescent rash and elevated ferritin levels. However, patients may also present with other clinical features, including sore throat, hepatomegaly, splenomegaly, lymphadenopathy and serositis.6
The disease course generally follows one of three patterns: 1) a singular, self-limited episode (i.e., monocyclic); 2) a pattern of continued flares with periods of remission (i.e., polycyclic); and 3) continued signs and symptoms with no periods of remission (i.e., chronic).3 At almost two years from initial diagnosis, our patient’s disease remains in remission; thus, he follows the monocyclic pattern.
There are no specific tests that confirm a diagnosis of AOSD; however, laboratory tests commonly show non-specific signs of generalized inflammation, including anemia, thrombocytosis, elevated inflammatory markers and significantly elevated ferritin. Of note, ferritin is usually markedly elevated and found to be much higher than in other autoimmune, infectious, inflammatory or neoplastic diseases. Higher levels of ferritin may also be an indicator of MAS.5
Click to enlarge.
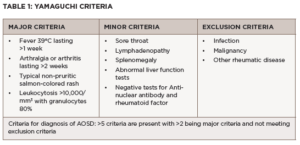
Although AOSD is largely a clinical diagnosis, clinicians can use the Yamaguchi criteria and Fautrel criteria to help classify it. As seen in Table 1, the Yamaguchi criteria require that five or more criteria be met, with at least two major criteria, and infection, malignancies and other rheumatic diseases ruled out.13 The Yamaguchi criteria has a sensitivity of 96.2% and a specificity of 92.1% in diagnosing AOSD.13
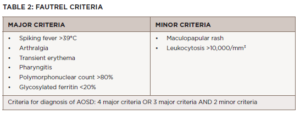
As seen in Table 2, the Fautrel criteria require at least four or more major criteria or three major criteria with two minor criteria be met. They have a sensitivity of 80.6% and specificity of 98.5%.4
Our patient’s disease characteristics fit both the Fautrel criteria and the Yamaguchi criteria because he had fever (>39ºC), leukocytosis with 96%, polymorphonuclear neutrophils, polyarthralgia/arthritis, abnormal liver function tests, pharyngitis and rash. In addition, his infectious and hematologic evaluations were negative, ruling out other causes of his presentation.
Click to enlarge.
The treatment aim for AOSD is to control inflammation and prevent end-organ damage, which can be assessed clinically and through serial measurement of inflammatory markers. The treatment initiated depends on disease severity. Patients are classified as having mild to moderate disease when symptoms are low grade, including mild fever, rash and arthralgias or arthritis. These patients may be treated with non-steroidal anti-inflammatory drugs (NSAIDs). However, NSAIDs alone fail to control symptoms in 80% of AOSD patients.9 If symptoms fail to improve after a two week trial of NSAIDs, glucocorticoids are recommended for management in mild cases.9