Patients with moderate to severe disease, as in the case of our patient, typically have signs of systemic illness, including debilitating polyarthritis, persistently elevated fever despite antipyretics, and serositis. In these cases, anakinra, an interleukin 1 receptor antagonist is recommended. Studies have shown that, in AOSD patients, anakinra was more likely to induce remission than DMARDs alone, and patients on anakinra were able to decrease or eliminate glucocorticoid use.12,7 Alternative medications for patients who are unable to tolerate anakinra include the other IL-1 inhibitors canakinumab and rilonacept, as well as the IL-6 inhibitor tocilizumab.14 Of note, only canakinumab is approved by the U.S. Food & Drug Administration for the treatment of AOSD.10
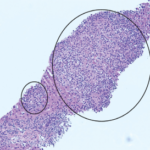
Numerous complications are associated with AOSD. Macrophage activation syndrome (MAS), found in up to 15% of AOSD patients, is one of the most severe complications, and the complication with the highest mortality rate.6 The mechanisms of MAS development in AOSD is unclear, but involves cytokine-induced hyperproliferation of activated CD8+ T lymphocytes and macrophages in the reticuloendothelial system.8 MAS is characterized by cytokine storm, hemophagocytosis and multi-system organ damage.2
Studies have shown that patients with AOSD complicated by MAS have a mortality rate of up to 52.9%, which is significantly higher than the mortality rate of AOSD alone, which is 9.5%.2 There are a few proposed scores for diagnosis of MAS, including the 2004-HLH criteria or H-Score, but the applicability of these tools in the context of AOSD remains unclear.
Because the diagnosis of AOSD with MAS is difficult, and the number of patients relatively low, little published literature on this topic exists. Treatment of MAS continues to evolve, with greater use of immunomodulators to help control the inflammation. Currently, high-dose intravenous glucocorticoids, which were administered to our patient and resulted in clinical improvement, remain a cornerstone of treatment.5
Even less is known about AOSD in people of African descent, with fewer than 10 cases discussed in the literature. Despite this small number of published reports, it is possible the condition is underdiagnosed. After all, there is a huge shortage of trained rheumatologists practicing within the continent of Africa. Additionally, classic textbook descriptions of AOSD describe a salmon-colored rash and in individuals with darker skin, this description may be misleading. Regardless, it is important to consider AOSD in patients of African descent who have a fever of unknown origin and significant hyperferritinemia.
 Cristina Romaniello, DO, is an internal medicine resident at Riverside Methodist Hospital in Columbus, Ohio. She graduated from West Virginia School of Osteopathic Medicine in 2020. She will pursue a career as a hospitalist following her residency.
Cristina Romaniello, DO, is an internal medicine resident at Riverside Methodist Hospital in Columbus, Ohio. She graduated from West Virginia School of Osteopathic Medicine in 2020. She will pursue a career as a hospitalist following her residency.