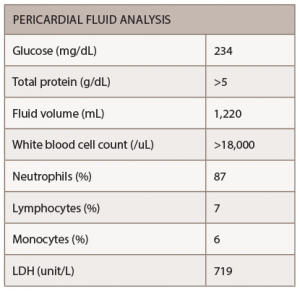
The patient underwent pericardiocentesis with the removal of 380 cc of bloody fluid. The findings of pericardial fluid are listed below (see Table 1).
The pericardial fluid showed no growth of bacterial or fungal cultures, and no acid-fast bacilli were seen, making mycobacterium tuberculosis unlikely. No evidence of malignant cells was found in the pericardial fluid. Colchicine with an anti-inflammatory medication were administered for the treatment of pericarditis.
Two days after the pericardiocentesis, the patient was transferred to the cardiac floor from the medical intensive care unit in stable condition. A repeat echocardiogram showed a left ventricle normal in size, with normal wall thickness and preserved systolic function, as well as minimal residual pericardial effusion.
Methotrexate was restarted after the infectious workup remained negative. The patient was discharged in stable condition, with no recurrence of symptoms on 0.6 mg of colchicine twice daily, 600 mg of ibuprofen three times daily and 20 mg of methotrexate weekly. He had a follow-up scheduled in two weeks with his rheumatologist when he would likely restart adalimumab.
Discussion
Pericardial involvement has been detected in a high percentage of RA patients in necropsy and echocardiographic studies (11–50%), but neither cardiac tamponade nor constrictive pericarditis is considered a common complication of the disease.5,2
Pericardial tamponade due to rheumatoid pericarditis can be a life-threatening complication.6 In 1990, Escalante et al. described 960 patients with RA who were followed over 11 years, and only five manifest cardiac compression.6 The male-to-female ratio of RA patients with tamponade (11:8) also differs from the normal RA population gender distribution, which typically trends toward women.6

Figure 1: A chest X-ray demonstrated moderate cardiomegaly with tortuous aorta.
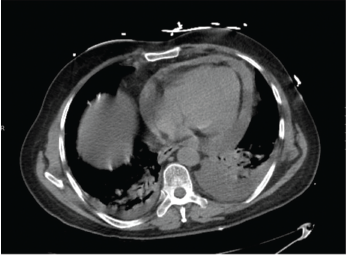
Figure 2: A computed tomography angiogram of the chest showed a moderate-sized complex pericardial effusion.
Cardiac compressions in rheumatoid pericarditis have also occurred in patients mostly older than 60 years with long-standing disease, according to most literature reported to date, including Nomeir et al. and Escalante et al.3,6 Symptomatic pericarditis often takes place in association with other extra-articular manifestations; rheumatoid factor is positive in 95% of the cases, and subcutaneous nodules are found in 35% of the patients.7
Diagnosis of Cardiac Tamponade
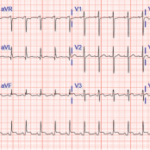
The diagnosis of cardiac tamponade can be made clinically by the finding of raised jugular venous pressure, distant heart sounds, hepatomegaly, ankle edema and pulsus paradoxus, and is substantiated by cardiac screening and echocardiography. In a review of 48 patients with RA, the authors described jugular vein distension in 60% and edema in 47%, although pulsus paradoxus or Kussmaul’s sign were uncommon.5
In the case of Mr. M, a muffled heart sound presented with no other physical examination finding of tamponade. The important diagnostic tool is aspiration of pericardial fluid. In the majority of reported cases the most frequent character of the fluid is hemorrhagic or serosanguinous. The fluid has the characteristic of exudate with high protein and lactate dehydrogenase.8 The sugar content of the fluid is either very low or absent.9 Cellular content is variable, but tends to be higher than 2,000.
In this case, pericardial fluid glucose was 234 mg/dL, but the protein was more than 5 g/dL. Most importantly, the cell count of more than 18,000 with the negative infectious and malignancy workup makes RA the most likely cause.
The infrequency of compressive pericardial diseases in RA limits the feasibility of studies to establish the effectiveness of any particular treatment strategy. Previous reports have demonstrated that treatment with non-steroidal anti-inflammatory drugs, corticosteroids and/or immunosuppressive drugs may be appropriate for RA-associated pericarditis.10
Systemic corticosteroids are often ineffective for the treatment of cardiac compression caused by rheumatoid pericarditis. Instead, percutaneous catheter drainage and surgical tube drainage are warranted.10 Rheumatoid pericardial effusions have responded to more intensive immunosuppression; however, some controversy exists on the effectiveness of tumor necrosis factor inhibitors on extra-articular manifestation.11
This is a rare complication that has historically occurred in patients with seropositive active rheumatoid arthritis, but its occurrence in patients with quiescent joint disease while on tumor necrosis factor inhibitors has been reported.11
Few studies have been conducted on RA as a cause for cardiac tamponade. No evidence-based therapeutic guidelines for rheumatoid pericarditis have been established yet. Further investigations are needed to make proper treatment recommendations.