At his one-month outpatient follow- up, his edema, headache, arthralgias, malaise, rash and diarrhea had all resolved. His cholesterol had normalized with statin therapy. Repeat urinalysis showed no blood and no protein, and the random urine-to-protein-creatine ratio had completely normalized (0.08 g/g Cr). His serum creatine declined to 1.2 mg/ dL. His inflammatory markers had also completely normalized (ESR 1 and CRP <0.5 mg/dL), as had his alkaline phosphatase and albumin.
Discussion
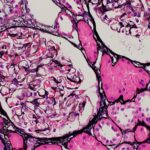
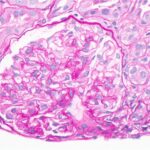
Searching PubMed, we identified only one case of co-infection with syphilis and parvovirus B19 mimicking lupus nephropathy, as in our patient.1 Parvovirus B19 and especially syphilis have been reported to cause the same histologic features of lupus nephritis—or so-called pseudolupus nephritis. Although the presence of C1q deposits is nearly pathognomonic for lupus nephritis, it can also be seen when parvovirus B19 causes kidney disease.1
Our patient’s positive ANA and full-house pattern on renal biopsy pointed toward lupus nephritis; however, the discordant findings of negative double-stranded DNA and anti-Smith antibodies, lack of cytopenias, normal complements and lack of other clinical features of systemic lupus erythematosus made us question the diagnosis.
Syphilis fit the clinical schema well—and it should be noted that our patient’s mild hepatitis, with isolated elevation of alkaline phosphatase, is very characteristic of syphilitic hepatitis.2 The presence of C1q deposition in the kidney prompted us to check for parvovirus B19 antibodies, which came back suggestive of acute infection. This likely explained his symptoms of malaise and arthralgias, as well as skin redness/rash (which was not appreciated on admission when we evaluated the patient, several weeks after symptom onset). Other masqueraders of lupus nephritis include HIV and infective endocarditis.
Syphilis has been historically referred to as the great mimicker given its heterogenous presentation.3,4 The three stages of infection are: primary, secondary and tertiary. Our patient likely had secondary infection, with rash and lymphadenopathy. Renal involvement can occur at any stage, from secondary to latent and tertiary. Both SLE and syphilis can have multi-system involvement.
This case illustrates the importance of thinking about infectious etiologies for glomerulonephritis and completing a thorough sexual history. Further, the diagnosis of lupus nephritis should be questioned when serologic and other laboratory markers (e.g., anti-Smith and double-stranded DNA antibodies, low complement levels, cytopenias) and clinical manifestations of lupus are absent, despite suggestive renal histology findings. The presence of C1q is nearly pathognomonic for lupus nephritis, but can also be seen when parvovirus B19 causes kidney disease.1 Parvovirus B19 and syphilis have been reported to cause the same histologic features of lupus nephritis.1,3,4-6