Initial urinalysis several weeks prior to admission showed 2–3+ protein, 2+ blood, and no casts. Proteinuria was quantified with random urine-to-protein-creatinine ratio, which was elevated at 5.65 g/g Cr. The ANA titer was 1:640 in nuclear coarse speckled pattern; tests for anti-Smith and double-stranded DNA antibodies were negative.
Serum complements were not low. A test for phospholipase A2 receptor (PLA2R) antibody was negative. Tests for human immunodeficiency virus (HIV) antigen and antibody, hepatitis B surface antigen and antibody, and hepatitis C antibody were negative. A test for RPR was positive (1:256), with a positive confirmatory syphilis total antibody test. Chlamydia and gonorrhea polymerase chain reaction testing returned negative. Tests for anti-phospholipid antibodies were negative.
The complete blood count test with differential was normal. Ferritin (408 ng/mL; RR: 12–300 ng/mL for men) and erythrocyte sedimentation rate (ESR) (56 mm/Hr; RR: 0–15 mm/Hr) were elevated; C-reactive protein (CRP) was just above the upper limit of normal (0.6 mg/dL; RR: <0.5 mg/dL).
Liver function tests revealed hypoalbuminemia (1.9 g/dL) and elevated alkaline phosphatase (413 U/L; RR: <129 U/L) and gamma-glutamyl transferase (872 U/L; RR: <61 U/L). Serum parvovirus B19 IgG (1.16 IV; RR: <0.90 IV) and IgM (1.97 IV; RR: <0.90 IV) were consistent with recently acquired infection.
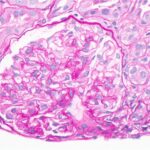
A renal biopsy was suggestive of classes II and V lupus nephritis; however, no crescents were identified (see Figure 1, opposite). Renal biopsy showed a combined (segmental) membranous and minimal mesangial pattern of glomerulonephritis with negative PLA2R antibody stain (see Figure 2, opposite). On immunofluorescence, glomeruli showed segmental, capillary loop and full-house pattern (positive for IgG, IgM, IgA, C3, C1q) co-staining (see Figures 3 and 4, this page). Spirochete stain was negative on immunohistochemistry.
Given the presence of persistent headache, along with neck tenderness and positive syphilis testing, a lumbar puncture with cerebrospinal fluid analysis was performed, which revealed normal cell count, negative gram stain, normal glucose and negative venereal disease research laboratory test.
Patient presented with nephrotic syndrome (i.e., nephrotic range: proteinuria, elevated cholesterol and edema), which improved during his hospitalization. He was treated with 30 mg of lisinopril daily and 40 mg of atorvastatin daily.
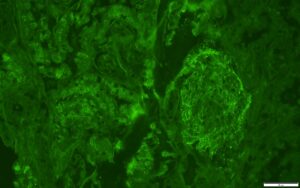
FIGURE 3: IMMUNOFLUORESCENCE IgG STAIN
IgG stain is positive in a granular pattern along capillary loop and rare mesangial areas.
(Click to enlarge.)
At his one-month outpatient follow-
up, his edema, headache, arthralgias, malaise, rash and diarrhea had all resolved. His cholesterol had normalized with statin therapy. Repeat urinalysis showed no blood and no protein, and the random urine-to-protein-creatine ratio had completely normalized (0.08 g/g Cr). His serum creatine declined to 1.2 mg/dL. His inflammatory markers had also completely normalized (ESR 1 and CRP <0.5 mg/dL), as had his alkaline phosphatase and albumin.
Discussion
Searching PubMed, we identified only one case of co-infection with syphilis and parvovirus B19 mimicking lupus nephropathy, as in our patient.1 Parvovirus B19 and especially syphilis have been reported to cause the same histologic features of lupus nephritis—or so-called pseudo-lupus nephritis. Although the presence of C1q deposits is nearly pathognomonic for lupus nephritis, it can also be seen when parvovirus B19 causes kidney disease.1