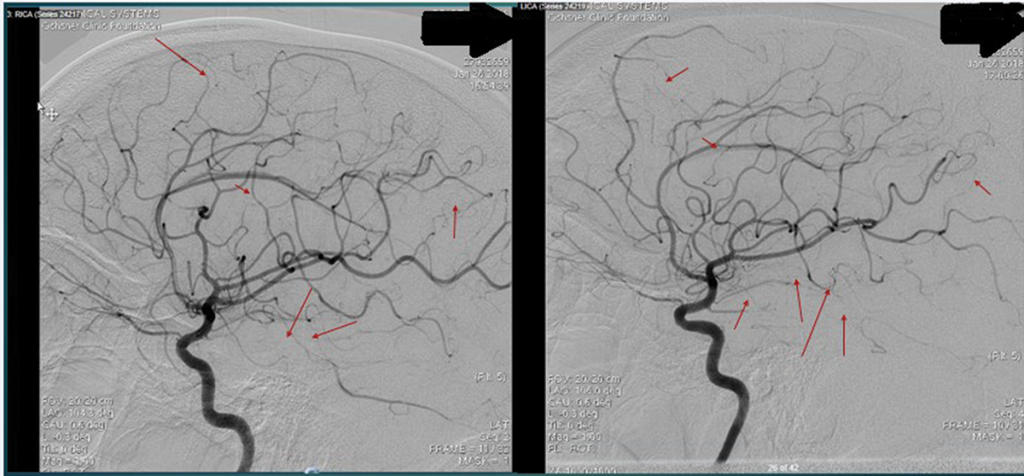
Figure 3 and Figure 4
An interventional radiology angiogram shows multifocal areas of distal intracranial artery narrowing.
Her rheumatoid factor was 22 IU/mL (normal: 0.0–15.0 IU/mL). Her C4 was elevated at 61 mg/dL (normal: 11–44 mg/dL). Her protein/creatinine ratio was 11.07 mg/mmol (normal: 0.00–0.20 mg/mmol).
Several diseases can mimic PACNS, including reversible cerebral vasoconstriction syndrome, premature intracranial atherosclerosis, fibromuscular dysplasia, secondary cerebral vasculitis, malignancy, infections …
Her renal function worsened after the angiogram, and she eventually required dialysis. A nephrologist was consulted and attributed her proteinuria and worsened renal dysfunction to underlying diabetes and contrast-induced nephropathy. A renal ultrasound was unremarkable.
The patient was initially started on 70 mg of prednisone daily. She was switched to pulse-dose steroids (1,000 mg methylprednisolone daily for three days) due to worsening neurologic status. Despite the pulse-dose steroids, the patient’s clinical progression continued to worsen. Repeat imaging showed evolving subacute infarcts.
After the patient was cleared by an infectious disease specialist and after discussion with the neurologist, the decision was made to administer renally dosed cyclophosphamide (415 mg/m2).
About one week after the cyclophosphamide infusion, the patient was able to follow commands and was attempting to state her name. She self-extubated and had an improved GCS of 15.
A brain biopsy showed lymphocytic vasculitis of uncertain etiology and remote cortical microinfarcts, with the affected
vessels showing a modest number of intramural lymphocytes and foci of chronic inflammatory cells within the adventitia, which were primarily positive for CD3 (see Figures 5–10, right). There was no evidence of granulomatous inflammation, fibrinoid necrosis of the vessel walls or infectious organisms. The patient was tapered to 15 mg methylprednisolone for eight days and eventually discharged to an inpatient rehab facility for follow-up with the rheumatologist, neurologist and nephrologist.

Figure 5: The leptomenigeal artery has significant narrowing due to cholesterol accumulation, and intramural and perivascular inflammatory infiltrates.
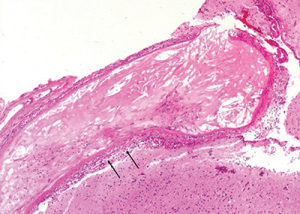
Figure 6: The image at higher magnification is highlighted to show the cholesterol accumulation, and intramural and perivascular inflammatory infiltrates.
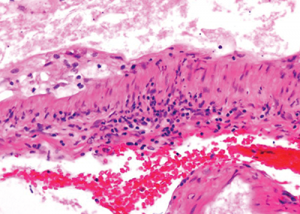
Figure 7: The image at even higher magnification shows the cholesterol accumulation, and intramural and perivascular inflammatory infiltrates.
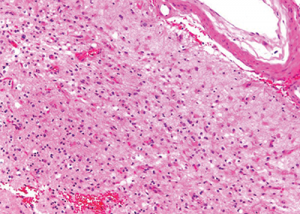
Figure 9: Subacute cortical microinfarct displaying loss of parenchyma and reactive gliosis.
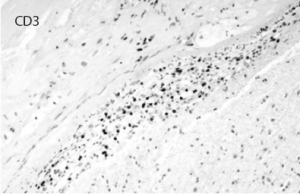
Figure 8: Immunostaining for CD3 highlights the inflammatory T cell population permeating the vascular wall. CD20 was mostly negative.