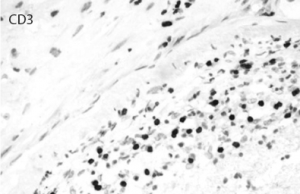
Courtesy of Maria-Beatriz Lopes, MD, University of Virginia Pathology
Discussion
PACNS is a poorly understood entity, and significant challenges remain for diagnosis and treatment. The pathogenesis is not well understood, and to date no evidence has been found to suggest a genetic predisposition. Various viral infections have been proposed as factors, such as varicella zoster virus, West Nile virus, Mycoplasma gallisepticum and HIV.6-14