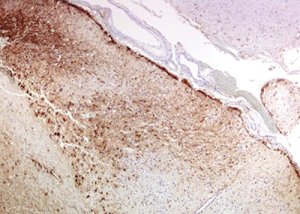
Figure 10: Immunohistochemistry for GFAP (glial fibrillary acidic protein) highlights the reactive gliosis of the subacute infarct.
The disease is considered in remission when the patient is stable and improved clinical and radiologic features are observed. Serial MRIs should be obtained to help in the assessment of disease activity, and clinicians may consider repeat CSF analysis.2
Efforts to limit accelerated atherosclerosis through aggressive control of diabetes, hypertension and dyslipidemia, as well as smoking cessation, is important. Routine vaccinations, osteoporosis prevention and prophylaxis for opportunistic infections should be included in treatment plan.2
The estimated mortality rate of PACNS varies between 10% and 17%. Hajj-Ali et al. found that survival correlated with the initial findings of infarcts and gadolinium-enhanced lesions on MRI.28
In the study analysis of 101 patients, Salvarani et al. reported 20% of patients with PACNS had moderate to severe disability, as assessed by the modified Rankin disability scores and the Barthel index, respectively.5
A literature review shows a Marburg variant of multiple sclerosis that presents with vasculitis and extensive demyelination; however, our patient did not have any areas of demyelination on pathological specimens, which makes this diagnosis less likely.29
A case of stroke occurring after initiation of interferon beta treatment for relapsing-remitting white matter disease has been reported.30 This case is similar to our patient, who had met criteria for multiple sclerosis and developed progression of neurological symptoms after initiation of the interferon-beta treatment. The question remains if her diagnosis of multiple sclerosis was accurate or if her symptoms at that time were related to undiagnosed CNS vasculitis.
Some evidence suggests autoimmune disease, especially vasculitis, worsens with interferon treatment. Thus, another concern is whether the interferon beta treatment was inappropriate and contributed to the severe cerebrovascular insufficiency.30
Conclusion
Diagnosis of PACNS remains a challenge and requires a high index of clinical suspicion, with appropriate workup to exclude other conditions. Further research needs to be done to improve our understanding of the etiology and pathogenesis of this disease, as well as our diagnosis and treatment approaches.
Gbemisola Olayemi, MD, is a graduate of the University of Pretoria, South Africa, and obtained her medical degree at the Medical University of the Americas, Charlestown, Nevis, West Indies. Her internal medicine residency was at Leonard J. Chabert Medical Center, Houma, La., and she is currently engaged in a rheumatology fellowship at Ochsner Clinic Foundation, New Orleans.
Eve Scopelitis, MD, joined the Department of Rheumatology at Ochsner Clinic in 2006. Prior to that she was professor of medicine and director of the Rheumatology Clinics at the Louisiana State University Health Sciences Center, New Orleans. Her medical degree was obtained at SUNY Upstate Medical Center in Syracuse, N.Y. She completed an internal medicine residency at Nassau County Medical Center, East Meadow, N.Y., and a fellowship in Rheumatology at the LSU Health Sciences Center, New Orleans.
Jerald M. Zakem, MD, joined the Department of Rheumatology at Ochsner Clinic in 2000. He is currently an Instructor for the University of Queensland at Ochsner Clinical School. Prior to that, he was a clinical assistant professor of medicine at the University of South Florida in Tampa. His medical degree was obtained at University of Louisville, Ky. He completed an internal medicine residency and a rheumatology fellowship at the University of South Florida.