Review of systems: He reported migratory polyarthritis, recent ocular pain and redness, and chronic low back pain and stiffness. The patient denied any skin rash, such as psoriasis; constitutional symptoms, including fever, chills, weight loss and night sweats; dactylitis; gastrointestinal or genitourinary symptoms; nasal discharge, crusting or bleeding; nasal or auricular chondritis; sinus or respiratory symptoms, such as cough, hemoptysis or shortness of breath; sore throat; numbness or tingling sensation in his extremities; recent infection, including sexually transmitted disease; or tick bite preceding his symptoms.
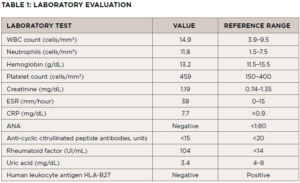
Physical examination & laboratory evaluation: Upon evaluation, the patient was afebrile (98ºF), had a blood pressure of 123/83 mmHg, a heart rate of 90 beats per minute and a normal respiratory rate.
He was well appearing and not in acute distress. He had clear sclera, without focal sinus tenderness, nasal crusting or deformity. His skin examination was normal, without evidence of psoriasis, nodules or purpuric rash. The lung auscultation was clear. The patient didn’t have any pitting edema in his lower extremities.
The musculoskeletal examination revealed no active synovitis in his joints, except for focal tenderness in both ankles without apparent effusion, and a Schober’s test was limited (i.e., 10–13 cm), without focal tenderness over his sacroiliac joints or the rest of his spine.
Differential Diagnoses
The differential diagnosis for migratory polyarthritis includes palindromic rheumatism, infectious processes, such as Lyme disease and viral infections, spondyloarthropathy, sarcoidosis, connective tissue disorders and vasculitides and paraneoplastic polyarthritis.3
Palindromic rheumatism: A rare inflammatory arthritis, palindromic rheumatism is characterized by recurrent attacks, manifesting as joint pain and swelling without chronic joint damage. Episodes are self-limited, resolving within a few hours to days. Patients with anti-cyclic citrullinated peptide (CCP) antibodies are at increased risk to progress into rheumatoid arthritis (RA) in up to 50% of cases.
Our patient presented with migratory polyarthritis without constitutional symptoms and had a positive rheumatoid factor (RF) test, which would put palindromic rheumatism high on the list of possible diagnoses. However, whereas episcleritis and scleritis are both reported in RA, a history of iritis is not usually a common symptom.4,5
Infectious causes: Viral and bacterial infections, such as parvovirus B19, may cause migratory polyarthritis by a reactive process. It may present as asymmetric oligoarthritis in children; in adults it tends to manifest as symmetrical polyarthritis.6 Hepatitis B can present prodromal symptoms, symmetrical polyarthritis and a positive RF test in up to 80% of cases.7