Paraneoplastic polyarthritis: A rare entity that has been described most in adenocarcinomas of the lungs and breasts, and as a hematological malignancy, paraneoplastic polyarthritis is characterized by migratory polyarthritis affecting primarily joints in the lower extremities, with the presence of RF and ANA in rare cases (20%).
Our patient was relatively young and had no constitutional symptoms or other symptoms concerning for indolent malignancy.13
Diagnosis & Clinical Course
Plain films of our patient’s sacroiliac joints and lumbar spine were unremarkable. Hepatitis, tuberculosis, Lyme disease and parvovirus tests were negative. His uric acid level was within normal limits at 3.4 mg/dL (reference range: 4–8 mg/dL).
Based on his symptoms and the presence of RF, the leading diagnosis was palindromic rheumatism. The patient was scheduled for a follow-up visit in two weeks to discuss his diagnosis and start treatment.
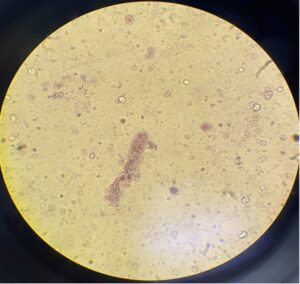
FIGURE 2. Microscopic examination of the patient’s urine sample shows one red blood cell cast. (Click to enlarge.)
Repeat laboratory tests prior to initiation of methotrexate revealed acute elevation of creatinine at 3.4 mg/dL, compared with his previous baseline of 1.19 mg/dL. A urinalysis showed +3 hemoglobin and +3 protein. Urine sedimentation showed many red blood cell casts (see Figure 2).
He was admitted for evaluation of acute kidney failure. Laboratory tests during admission revealed the presence of C-ANCA and proteinase-3 antigen >8 (normal range < 1) and negative cryoglobulin and anti-glomerular basement membrane (GBM) antibodies.
Chest radiography was unrevealing, without hilar adenopathy. Computed tomography (CT) showed small subpleural nodules in the right lower and left upper lobes. CT of his sinus without contrast showed a clear mastoid and minimal mucosal thickening of the maxillary sinuses without acute sinusitis.
His ophthalmologic exam was consistent with episcleritis and possible mild anterior scleritis.
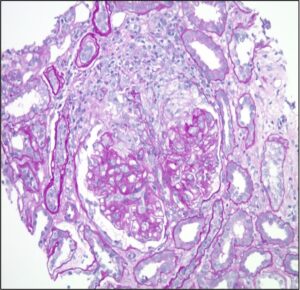
FIGURE 3. Kidney biopsy reveals pauci-immune necrotizing and crescentic glomerulonephritis. (Click to enlarge.)
He underwent right-sided kidney biopsy, and the pathology was consistent with pauci-immune necrotizing and crescentic glomerulonephritis with mild interstitial fibrosis (see Figure 3).
The patient was diagnosed with GPA and was administered pulse-dose methylprednisolone and four weekly infusions of rituximab in a dosage of 375 mg/m2 of body surface area.
Discussion
This case emphasizes the difficulties of early systemic vasculitides diagnosis and detection, which are always essential to avert serious morbidity and mortality.
AAV has a wide range of clinical manifestations, from single-organ limited to fulminant multi-system disease. Almost any organ can be affected, although the upper airways, lungs, kidneys, eyes and peripheral nerves are the most-often involved organs.

