She was diagnosed with AOSD based on clinical features of daily fevers for more than a week, arthralgias for more than two weeks, leukocytosis (>10,000 with predominant polymorphonuclear leukocytes), elevated liver function tests (LFTs) and inflammatory markers with very high ferritin, a negative infectious evaluation, no evidence of malignancy and positive skin biopsy. She was classified as having AOSD based on the Yamaguchi criteria (see Table 1).
She was started on 100 mg of anakinra daily, experiencing complete resolution of her clinical symptoms and rapid improvement of her laboratory abnormalities, with down-trending ferritin and normalized WBC in a week.
She was discharged on 40 mg of prednisone daily with a taper due to denial of insurance coverage for anakinra, and her symptoms reappeared during the prednisone taper. Ultimately, anakinra was approved by her insurance company. Due to injection-site reactions, she was switched to monthly infusions of 8 mg/kg of tocilizumab.
At one year follow-up, the patient remained in clinical remission, with improved residual hyperpigmentation. Twenty months after the diagnosis of AOSD, she was diagnosed with ductal carcinoma of the breast.
Discussion
The most common rash associated with AOSD is a salmon-colored, non-pruritic, evanescent, maculopapular rash involving the extremities and trunk, usually accompanying the fever and disappearing when the fever subsides. The histopathology of the evanescent rash is nonspecific and may be more useful for excluding alternative diagnoses, such as drug reactions.
Complicating matters is that the skin rash of AOSD may also present as persistent, pruritic, hyperpigmented papules, plaques or linear pigmentation. These lesions are commonly found on the trunk and extensor surface of the extremities, and often resemble lesions associated with dermatomyositis.4–10 The histopathology reveals distinctive features, including dyskeratosis, necrotic keratinocytes, parakeratosis primarily observed in the superficial layers of the epidermis, without concurrent basilar dyskeratosis, and a sparse, superficial dermal infiltrate, often containing neutrophils or less frequently lymphocytes, without vasculitis.4,6,10 This rash may be associated with more severe disease and a worse prognosis, consistent with our case; our patient had an incomplete response to high-dose prednisone but responded well to interleukin (IL) 1 and IL-6 blockade.10,11
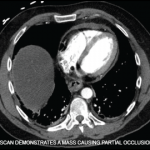
A further diagnostic challenge associated with AOSD is that malignancies can present with symptoms that resemble AOSD, and also that AOSD may rarely be a paraneoplastic phenomenon that precedes the diagnosis of malignancy.12 In a systematic literature review conducted by Hofheinz et al., 36 cases of AOSD associated with malignancy were reported, with half of them diagnosed with solid tumors and the other half with hematologic malignancies.13 The median time from AOSD diagnosis to the malignancy diagnosis was nine months. Among cases with solid tumors, the most frequent types were ductal breast cancer (n=4) and non-small cell lung cancer (n=3). Sixty-seven percent of the patients with solid cancer had metastatic involvement at the time of diagnosis. It is unclear in this case how the AOSD was related to the subsequent diagnosis of ductal carcinoma.