Positron emission tomography-computed tomography (PET-CT) imaging demonstrated infiltrative tissue at the pulmonary artery outflow tract and increased metabolic activity in the proximal pulmonary arteries (see Figures 3 and 4).
Laboratory tests were notable for a positive ANCA at a titer of 1:640, P-ANCA pattern, and with a positive immunoassay for myeloperoxidase (MPO) >8. Anti-nuclear antibody (ANA), extractable nuclear antigen (ENA), double-stranded DNA (dsDNA) and eosinophil counts were negative or normal. Urinalysis revealed microscopic hematuria (2+ blood, >50 red blood cells per high-power field) with normal protein levels and protein-creatinine ratio. Other laboratory results, including white blood cell count, hemoglobin, liver function tests and creatinine, were unremarkable.
The patient was started on 60 mg of prednisone daily, 30 mg of avacopan twice daily and 1 g of rituximab every two weeks for two doses. She reported symptomatic improvement, including resolution of dyspnea, rash, sinus symptoms and constitutional complaints.
A ventilation-perfusion scan demonstrated diffuse and focal areas of decreased perfusion in the left lung. Right heart catheterization (RHC) confirmed proximal right pulmonary artery stenosis, with a peak gradient of 24 mmHg, and pulmonary artery systolic pressure (PASP) of 72 mmHg, with a mean pulmonary artery pressure (mPAP) of 32 mmHg. Left and right heart filling pressures and cardiac output were normal.
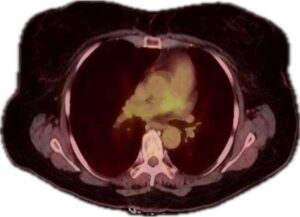
Figure 3 (transverse view): PET-CT demonstrating increased metabolic activity in the proximal pulmonary arteries. (Click to enlarge.)
With treatment, the patient experienced symptomatic improvement as prednisone was tapered. A follow-up PET scan showed reduced inflammation in the pulmonary artery outflow tract and proximal pulmonary arteries. Repeat chest CT angiography was stable, and pulmonary function tests and CT imaging of the sinuses were normal.
Subsequently, she underwent bilateral pulmonary artery stenting, leading to a significant improvement in pulmonary artery systolic pressure (PASP) from 72 mmHg to 35 mmHg. She continued to do well clinically on follow-up.
Discussion
The involvement of large vessels, such as the pulmonary artery, in ANCA-associated vasculitis is a rare but clinically significant manifestation. Pulmonary artery involvement can lead to such complications as progressive stenosis, pulmonary hypertension and right-side heart failure.
A multi-center case-control study by Monghal et al. found the aorta was the most commonly affected vessel, with involvement in 69% of cases. Other affected vessels included the supra-aortic trunks (35%), lower-limb arteries (19%), mesenteric arteries (19%), renal arteries (15%) and upper-limb arteries (8%).3 Pulmonary artery involvement was not noted in this cohort. However, multiple case reports have documented pulmonary artery involvement in ANCA-associated vasculitis, indicating that although rare, it is a recognized clinical entity.

