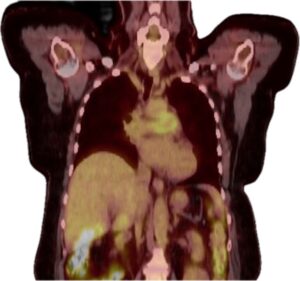
Figure 4 (coronal view): PET-CT demonstrating increased metabolic activity in the proximal pulmonary arteries. (Click to enlarge.)
We conducted a literature review using the following search terminology: (“Granulomatosis with Polyangiitis” [MeSH] OR “Microscopic Polyangiitis” [MeSH] OR “Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis” [MeSH] OR “ANCA-associated vasculitis” OR “Wegener’s granulomatosis” or myeloperoxidase antibody OR proteinase 3 antibody) AND (“Pulmonary Artery” [MeSH] OR “Pulmonary Artery Stenosis” [MeSH] OR “Pulmonary Arteritis” OR “pulmonary artery vasculitis”).
This search yielded 45 results, from which we reviewed eight relevant articles.2,4-10 Including our patient, we reviewed a total of nine patients.
Table 1 (see below) summarizes reported cases, highlighting the diverse presentations, diagnostic challenges and therapeutic approaches associated with pulmonary artery stenosis in ANCA-associated vasculitis.
The age of affected patients ranged from 22 to 62 years, with a majority being women (78%). Most patients had classical ENT (ear, nose and throat) symptoms prior to the diagnosis of pulmonary stenosis, with duration ranging from three to six years. In some cases, pulmonary artery stenosis was synchronous with the diagnosis of GPA; in one patient, it was discovered 21 years after the diagnosis of GPA.
Diagnosis relied on clinical features, serological tests, imaging and histopathology. C-ANCA with anti-proteinase 3 (PR3) antibody was detected in four of seven patients. P-ANCA with MPO antibody was detected in three of seven patients; in two cases, this information was unavailable. Imaging modalities, such as CT pulmonary angiogram, conventional angiogram, echocardiography and FDG-PET were pivotal. Angiograms were mainly helpful in diagnosing luminal abnormalities; FDG-PET and cardiac MRI were useful for detecting vessel wall abnormalities, and ECHO/RHC for evaluating pulmonary hypertension.
The pulmonary artery lesions typically presented as severe stenosis involving the proximal or main branches of the pulmonary arteries, although distal involvement was also noted in one patient.2 Among the nine cases reviewed, four confirmed the diagnosis with a histopathology showing pulmonary arteritis secondary to GPA.4,6,7,10
A case report by Doyle et al. noted that imaging of the pulmonary arteries with conventional imaging modalities, such as CTPA (computed tomography pulmonary angiography) or conventional pulmonary angiogram, is identical between arteritis and chronic thromboembolic disease and often needs a histopathological diagnosis for confirmation, which can unfortunately be challenging due to surgical complications and isn’t always obtained.7 Use of multimodal imaging techniques, including CTPA, conventional angiogram, echocardiogram and FDG-PET can be useful in diagnosing pulmonary stenosis and assessing the severity of pulmonary hypertension.

