
Figure 1. At her initial evaluation, the patient presented with a bullous lesion on her left foot.
Acute febrile neutrophilic dermatosis, or Sweet syndrome, is an inflammatory disease that classically presents with fever, leukocytosis and tender, erythematous plaques characterized by neutrophilic infiltrates on biopsy. Sweet syndrome has been reported in association with several autoimmune diseases, including inflammatory bowel disease, systemic lupus erythematous, rheumatoid arthritis and sarcoidosis.1 Here, we discuss a case of Sweet syndrome as the initial presentation of Crohn’s disease, manifesting with bullous skin lesions, splenic cysts, acute arthritis and an intraosseous calcaneal lesion.
Case Presentation
An 18-year-old woman was transferred to our institution for evaluation of persistent fevers and polyarticular arthritis that began 10 days prior to transfer. Symptoms began with pain in her bilateral ankles and associated blisters on the lateral malleoli. She then developed swelling in her feet, with fixed internal rotation, and was evaluated at a local hospital due to the inability to bear weight.
She was admitted to a hospital when she presented with this pain and night sweats, and was found to be febrile. Subsequently, she developed right hand pain and swelling. Prior to admission, she was otherwise healthy but reported three episodes of abdominal pain with hematochezia, the first occurring two months prior to admission. She reported unintentional weight loss of 10 lbs., dyspnea with rest and exertion, and 10 days of abdominal pain.
On physical exam, her vital signs included a temperature of 102.4º F, a heart rate of 112 beats per minute, and her blood pressure and oxygen saturation were within normal parameters. The musculoskeletal exam was notable for pitting edema of her right hand. Scattered metacarpophalangeal and proximal interphalangeal joints were tender without obvious synovitis, but the joint exam was impaired by the presence of edema.
She also had pitting edema in both feet, which were diffusely tender to palpation (see Figure 1). Both feet were internally rotated, and her range of motion at the ankles was limited by pain. Large bullae were present on both lateral malleoli, with purulent drainage from the lesion on the left lateral malleolus. The patient was tender to palpation at the left upper quadrant of the abdomen. The remainder of her exam was unremarkable.
Laboratory results revealed a leukocytosis of 19.4 K/μL with 81% granulocytes (reference range [RR]: 3.5–10.5 K/μL) and thrombocytosis of 810 K/μL (RR: 150–400 K/μL), C-reactive protein (CRP) of 287.5 mg/L (RR: <8.1 mg/L) and erythrocyte sedimentation rate (ESR) of 102 mm/hr (RR: 0–20 mm/hr). Basic metabolic panel and liver function tests were unremarkable.
Laboratory testing was remarkable for the presence of an atypical anti-neutrophil cytoplasmic antibody (ANCA). Tests for rheumatoid factor, anti-cyclic citrullinated peptide antibody, anti-nuclear antibody, antibodies against extractable nuclear antigens and anti-double-stranded deoxyribonucleic acid antibody were negative. An extensive infectious evaluation for bacterial, viral, fungal and mycobacterial etiologies, including cultures of the bullous skin lesions, was negative. Both a transthoracic and transesophageal echocardiogram were negative for vegetations.
A computed tomography (CT) scan of her chest, abdomen and pelvis revealed a left, lower lobe consolidation in her lung with a large left pleural effusion, and splenomegaly with numerous large cystic lesions. The largest splenic lesion was a partially septated, fluid-filled lesion that measured 9.3×7.3×5.4 cm. These lesions were significantly enlarged from an earlier CT scan completed two months prior to further evaluate for potential causes of hematochezia. Aspirations of both the pleural effusion and the splenic lesions failed to demonstrate infectious etiologies, but demonstrated numerous neutrophils.
Magnetic resonance imaging (MRI) of both feet demonstrated multiple, mildly complex, T2 hyperintense, loculated, intramuscular collections tracking along multiple tendons, with the largest one measuring 3.0×1.2×3.8 cm (see Figure 2A). It also showed a 1.0 cm calcaneal intraosseous collection concerning for an abscess. A punch biopsy of the bullous lesion on her right foot revealed mixed perivascular and interstitial inflammation with neutrophils in the epidermis, dermis and subcutaneous tissue (see Figure 3).
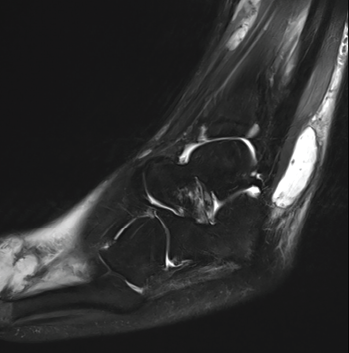
Figure 2A: This MRI of the patient’s left ankle (sagittal view) demonstrates a T2 hyperintense complex fluid collection within the posterolateral subcutaneous tissues overlying and coursing along the peroneus tendon and muscles. The collection measures 3.0×1.2×3.8 cm. This image also partly demonstrates a lobulated cystic-appearing fluid collection within the dorsal soft tissues of the forefoot.
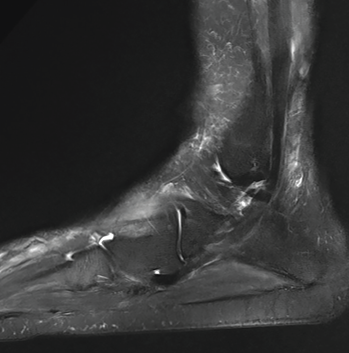
Figure 2B: A later MRI demonstrates resolution of previously seen fluid collections after treatment with corticosteroids.
She was diagnosed with Sweet syndrome.
At this point, the patient had already completed several days of broad-spectrum antibiotics without resolution of fevers or improvement in symptoms. She received 50 mg of intravenous methylprednisolone for three days, with immediate signs of clinical improvement. She defervesced with a significant reduction in her CRP to 45.8 mg/L (RR: <8.1 mg/L). Her right hand pain and swelling, in addition to her skin lesions, rapidly improved with treatment. Her foot pain and swelling slowly improved, and she transitioned to oral prednisone.
Given the episode of hematochezia two months prior to admission, a gastroenterologist was consulted for a colonoscopy to identify an underlying cause of Sweet syndrome. A colonoscopy was performed and revealed perianal bullae and erythematous, granular and inflamed mucosa in the ascending colon and cecum.
Biopsies showed active colitis in the right colon, patchy active inflammation in the transverse colon and rectum, and crypt abscesses in the rectum. No granulomas were identified, and a diagnosis of Crohn’s disease was made.
The patient was discharged home with a prolonged prednisone taper and plans to follow up with the gastroenterology and rheumatology services as an outpatient. Over the next two months, the patient began treatment with adalimumab for Crohn’s disease and completed her prednisone taper. A repeat MRI of her feet was performed three months after discharge and showed complete resolution of the abscesses (see Figure 2B).
Discussion
Sweet syndrome, or acute febrile neutrophilic dermatosis, is a rare inflammatory disorder belonging to the family of neutrophilic dermatoses. The syndrome is characterized by fevers, sudden onset of painful erythematous plaques or nodules and dense neutrophilic infiltrates on biopsy. The three subtypes of Sweet syndrome are classic Sweet syndrome, malignancy-associated Sweet syndrome and drug-induced Sweet syndrome.


