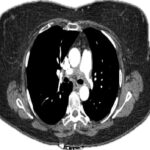
Figure 2. Coronal section from CTA of the abdomen and pelvis taken on hospital day
11 highlighting IMA involvement in SAM. The arrow points to proximal IMA thrombus with multifocal severe narrowing. The asterisk represents an area of large volume pneumoperitoneum resulting from perforation of the distal transverse colon. The arrowhead
corresponds to partially visualized large retroperitoneal hematoma. (Click to enlarge.)
Laboratory testing for hepatitis B and C, HIV and tuberculosis returned negative. ANCA, ANA, ENA tests were negative and no cryoglobulins were detected. A CRP was elevated at 168 mg/L and complement 3 protein was low at 69 mg/dL. The patient received intravenous methylprednisolone at 500 mg every 12 hours for three days, followed by 48 mg daily. He was successfully extubated after nine days.
A repeat staging CT angiogram of the abdomen showed a new large pneumoperitoneum with a large volume of free fluid suspicious for perforated viscus (see Figure 2). The patient was brought to the operating room where greater than 5 L of old clot were seen in the abdomen, along with signs of ischemia and perforation of the distal transverse colon and questionable perfusion to the left colon.
The colon was resected from the mid transverse to proximal rectum and an end side colostomy was formed. Histopathology from the resected bowel segments showed necrosis of the vessel wall in one of the branches of the mesenteric artery, along with degenerative changes in the smooth muscle. The findings were deemed consistent with SAM (see Figures 3a and 3b). There was no evidence of vasculitis in the vessels sampled away from the perforation site.
The patient was tapered off steroids following the results of the biopsy. Additional vessel imaging revealed a 1.1 cm aneurysm of the right internal carotid artery. His hospital course was complicated by acute kidney injury requiring intermittent hemodialysis, and critical illness myopathy. His condition slowly improved, and he was discharged to a rehabilitation facility after hospital day 27. He returned to the emergency department three months later with similar symptoms. A repeat CT of the abdomen showed arterial blush and venous pooling in the region of the pancreatic head. Angiography found multiple pseudoaneurysms throughout the mesenteric vasculature. Coil embolization was performed on a large pseudoaneurysm arising from the superior mesenteric artery.
SAM Introduction
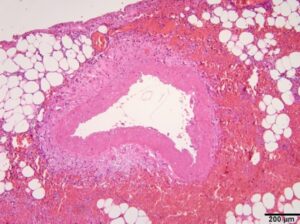
Figure 3a. Sampling of arteries in viable areas of the colon resection demonstrates variable degrees of necrosis of the arterial wall. The H&E section (x10 objective) of one artery shows fibrinoid necrosis of the tunica media involving the entire circumference of the artery. There is no significant inflammatory infiltrate, arguing against a vasculitic process. (Click to enlarge.)