Discussion
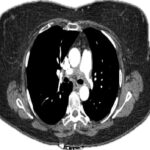
Rare, non-atherosclerotic, non-inflammatory arteriopathies, vEDS and SAM are potentially life-threatening, as indicated in our cases. Both conditions can present with imaging findings that mimic PAN and can similarly lead to devastating complications including aneurysm formation, dissection and spontaneous vascular rupture.
Despite the potential similarities with regards to presentation, vEDS and SAM are managed differently than PAN. Given immune-mediated underpinnings, PAN typically requires treatment with systemic glucocorticoids and immunosuppressants, such as mycophenolate mofetil or methotrexate. In severe, organ- or life-threatening disease, cyclophosphamide may be used.35 In contrast, management of vEDS and SAM do not involve immunosuppression and are primarily preventive and supportive—including regular vascular surveillance, strict blood pressure control and lifestyle modifications (e.g., avoidance of unnecessary invasive procedures and trauma). In the setting of complications, such as hemorrhage, ischemia or rapid evolution of vascular defects, surgery, endovascular embolization or stenting may be required.18,28
Ultimately, vEDS and SAM should be considered in the differential for patients presenting with clinical features or imaging suggestive of PAN, especially in the absence of systemic symptoms, because accurate diagnosis can have profound impacts on management.
 Shane Murray, BMBS, RhMSUS, obtained his medical degree at the University of Limerick, Ireland. He completed an internal medicine residency at Mount Sinai Morningside & Mount Sinai West Hospitals, New York, and a rheumatology fellowship at Columbia University Irving Medical Center, N.Y. He joined the Department of Rheumatology at the Yale School of Medicine in 2024.
Shane Murray, BMBS, RhMSUS, obtained his medical degree at the University of Limerick, Ireland. He completed an internal medicine residency at Mount Sinai Morningside & Mount Sinai West Hospitals, New York, and a rheumatology fellowship at Columbia University Irving Medical Center, N.Y. He joined the Department of Rheumatology at the Yale School of Medicine in 2024.
 Zhe Ran Duan, MD, PhD, obtained her medical degree at Weill Cornell Medical College, New York. She completed an anatomic pathology residency at Columbia University Irving Medical Center, New York, and is currently completing a surgical pathology fellowship there.
Zhe Ran Duan, MD, PhD, obtained her medical degree at Weill Cornell Medical College, New York. She completed an anatomic pathology residency at Columbia University Irving Medical Center, New York, and is currently completing a surgical pathology fellowship there.
 Daniel DeMizio, MD, obtained his medical degree at Albert Einstein College of Medicine in New York. He completed his internal medicine residency at Mount Sinai Hospital in New York and his rheumatology fellowship at Columbia University Irving Medical Center, N.Y. He has served as chief of rheumatology at Richmond University Medical Center, New York, since 2023.
Daniel DeMizio, MD, obtained his medical degree at Albert Einstein College of Medicine in New York. He completed his internal medicine residency at Mount Sinai Hospital in New York and his rheumatology fellowship at Columbia University Irving Medical Center, N.Y. He has served as chief of rheumatology at Richmond University Medical Center, New York, since 2023.
References
- Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1–11.
- Pagnoux C, Seror R, Henegar C, et al. Clinical features and outcomes in 348 patients with polyarteritis nodosa: a systematic retrospective study of patients diagnosed between 1963 and 2005 and entered into the French Vasculitis Study Group Database. Arthritis Rheum. 2010;62(2):616–626.
- Pontes T de C, Rufino GP, Gurgel MG, et al. Fibromuscular dysplasia: a differential diagnosis of vasculitis. Rev Bras Reumatol. 2012;52(1):70–74.
- Filippone EJ, Foy A, Galanis T, et al. Segmental arterial mediolysis: report of 2 cases and review of the literature. Am J Kidney Dis Off J Natl Kidney Found. 2011;58(6):981–987.
- Slavin RE, Inada K. Segmental arterial mediolysis with accompanying venous angiopathy: a clinical pathologic review, report of 3 new cases, and comments on the role of endothelin-1 in its pathogenesis. Int J Surg Pathol. 2007;15(2):121–134.
- Slavin RE, Cafferty L, Cartwright J. Segmental mediolytic arteritis. A clinicopathologic and ultrastructural study of two cases. Am J Surg Pathol. 1989;13(7):558–568.
- Slavin RE, Saeki K, Bhagavan B, et al. Segmental arterial mediolysis: a precursor to fibromuscular dysplasia? Mod Pathol Off J U S Can Acad Pathol Inc. 1995;8(3):287–294.
- Inada K, Maeda M, Ikeda T. Segmental arterial mediolysis: unrecognized cases culled from cases of ruptured aneurysm of abdominal visceral arteries reported in the Japanese literature. Pathol Res Pract. 2007;203(11):771–778.
- Chao CP. Segmental arterial mediolysis. Semin Interv Radiol. 2009;26(3):224–232.
- Slavin RE. Segmental arterial mediolysis: course, sequelae, prognosis, and pathologic-radiologic correlation. Cardiovasc Pathol Off J Soc Cardiovasc Pathol. 2009;18(6):352–360.
- Alhalabi K, Menias C, Hines R, et al. Imaging and clinical findings in segmental arterial mediolysis (SAM). Abdom Radiol N Y. 2017;42(2):602–611.
- Tameo MN, Dougherty MJ, Calligaro KD. Spontaneous dissection with rupture of the superior mesenteric artery from segmental arterial mediolysis. J Vasc Surg. 2011;53(4):1107–1112.
- LaBerge JM, Kerlan RK. SCVIR Annual Meeting Film Panel Session: case 3. Segmental arterial mediolysis (SAM) resulting in spontaneous dissections of the middle colic and left renal arteries and occlusion of the SMA. Society of Cardiovascular & Interventional Radiology. J Vasc Interv Radiol. 1999;10(4):509–513.
- Obara H, Matsumoto K, Narimatsu Y, et al. Reconstructive surgery for segmental arterial mediolysis involving both the internal carotid artery and visceral arteries. J Vasc Surg. 2006;43(3):623–626.
- O’Shea JP, Gordon S, Horak R, et al. Segmental Arterial Mediolysis (SAM) Leading to Chronic Renal Insufficiency. Int J Nephrol Renov Dis. 2021;14:117–123.
- de Sa DJ. Coronary arterial lesions and myocardial necrosis in stillbirths and infants. Arch Dis Child. 1979;54(12):918–930.
- Lie JT, Berg KK. Isolated fibromuscular dysplasia of the coronary arteries with spontaneous dissection and myocardial infarction. Hum Pathol. 1987;18(6):654–656.
- Kalva SP, Somarouthu B, Jaff MR, et al. Segmental arterial mediolysis: clinical and imaging features at presentation and during follow-up. J Vasc Interv Radiol. 2011;22(10):1380–1387.
- Hamby WB. Spontaneous subarachnoid hemorrhage of aneurysmal origin; factors influencing prognosis. J Am Med Assoc. 1948;136(8):522–528.
- Ohtoh T, Ono Y, Iwasaki Y, et al. Non-traumatic recurrent dissection and its spontaneous repair in the circle of Willis: report of two autopsy cases. Neuropathology. 2003 Sep;23(3):195–198.
- Superti-Furga A, Gugler E, Gitzelmann R, et al. Ehlers-Danlos syndrome type IV: a multi-exon deletion in one of the two COL3A1 alleles affecting structure, stability, and processing of type III procollagen. J Biol Chem. 1988;263(13):6226–6232.
- Mizuno K, Boudko S, Engel J, et al. Vascular Ehlers-Danlos Syndrome Mutations in Type III Collagen Differently Stall the Triple Helical Folding. J Biol Chem. 2013;288(26):19166–19176.
- Frank M, Albuisson J, Ranque B, et al. The type of variants at the COL3A1 gene associates with the phenotype and severity of vascular Ehlers-Danlos syndrome. Eur J Hum Genet. 2015;23(12):1657–1664.
- Pepin MG, Schwarze U, Rice KM, et al. Survival is affected by mutation type and molecular mechanism in vascular Ehlers-Danlos syndrome (EDS type IV). Genet Med. 2014 Dec;16(12):881–888.
- Malfait F, De Paepe A. The Ehlers-Danlos syndrome. Adv Exp Med Biol. 2014;802:129–143.
- Pepin M, Schwarze U, Superti-Furga A, et al. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med. 2000;342(10):673–680.
- Chu LC, Johnson PT, Dietz HC, et al. Vascular complications of Ehlers-Danlos syndrome: CT findings. AJR Am J Roentgenol. 2012 Feb;198(2):482–487.
- Oderich GS, Panneton JM, Bower TC, et al. The spectrum, management and clinical outcome of Ehlers-Danlos syndrome type IV: a 30-year experience. J Vasc Surg. 2005;42(1):98–106.
- Molloy ES, Langford CA. Vasculitis mimics. Curr Opin Rheumatol. 2008;20(1):29–34.
- Michael M, Widmer U, Wildermuth S, et al. Segmental arterial mediolysis: CTA findings at presentation and follow-up. AJR Am J Roentgenol. 2006;187(6):1463–1469.
- Begelman SM, Olin JW. Fibromuscular dysplasia. Curr Opin Rheumatol. 2000;12(1):41-47.
- McCormack LJ, Poutasse EF, Meaney TF, et al. A pathologic-arteriographic correlation of renal arterial disease. Am Heart J. 1966;72(2):188–198.
- Harrison EG, Hunt JC, Bernatz PE. Morphology of fibromuscular dysplasia of the renal artery in renovascular hypertension. Am J Med. 1967;43(1):97–112.
- Olin JW, Froehlich J, Gu X, et al. The United States Registry for Fibromuscular Dysplasia: Results in the first 447 patients. Circulation. 2012;125(25):3182–3190.
- Chung SA, Gorelik M, Langford CA, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Polyarteritis Nodosa. Arthritis Care Res. 2021 Aug; 73(8):1061–1070.