Dr. Oddis reviewed the two classifications of idiopathic inflammatory myopathy: clinical groups, including adult and juvenile, and serologic groups, or those with autoantibodies. The second group includes myositis-specific autoantibodies. Categories of myositis-specific autoantibodies include anti-synthetases, which present with acute and aggressive onset with pulmonary symptoms such as interstitial lung disease. Other symptoms include high fever, inflammatory arthritis, and sometimes deforming arthritis of the hands. These patients are often thought to have pneumonia and/or rheumatoid arthritis, said Dr. Oddis. The pulmonary involvement can be life threatening.
There is very little evidence-based treatment for pharmacologic therapy of idiopathic inflammatory myopathy, according to Dr. Oddis. Current treatment may include corticosteroids, immunosuppressive agents, combination regiments, intravenous immunoglobulin, and biologic agents such as anti-TNF agents, monoclonal anti-B cell agents, and monoclonal anti-complement agents.
A current NIH trial is assessing the efficacy of rituximab in polymyositis and DM, said Dr. Oddis.
Childhood Vasculitis Update
Rayfel Schneider, MD, associate professor of pediatrics at the University of Toronto in Ontario and head of rheumatology at the Hospital for Sick Children there, presented “Pediatric Vasculitis,” a review of the current classification of childhood vasculitis, diagnostic pitfalls, and new treatment developments.
Beginning with the 2005 practical classification for childhood vasculitis—which Dr. Schneider calls “a work in progress”—he reviewed large-vessel, medium size–vessel, and small-vessel vasculities. He then focused on Wegener’s granulomatosis (WG)—a small-vessel vasculitis—and primary angiitis of the central nervous system (PACNS) in children, because, he says, “we’re seeing an increasing number of patients with isolated vasculitis of the CNS and we’ve done some work in that area.”
Dr. Schneider outlined recent research on Wegener’s granulomatosis in children, pointing out common symptoms including fever, arthralgia, and weight loss; glomerulonephritis; upper airway disease; and pulmonary disease. Less common symptoms include eye involvement, skin vasculitis, arthritis, and venous thrombosis.
“Wegener’s in children is more common in females,” Dr. Schneider says. “Think about Wegener’s in children with ‘atypical’ [Henoch-Schoenlein purpura]. Constitutional symptoms and upper airway, pulmonary, and renal involvement are all very common at presentation, and some patients may present with [deep venous thrombosis].”
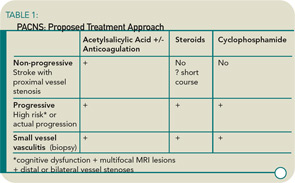
Dr. Schneider then reviewed the proposed diagnostic criteria for PACNS, which include newly acquired neurological deficit, angiographic and/or histological features of CNS vasculitis, and no evidence of a systemic condition associated with these findings. Mimics must also be excluded.
He stressed that PACNS is a heterogeneous disease. It can present with acute stroke or diffuse neurological deficits—or with both. Permanent neurological deficits are frequent.