-
Gustavo Frazao / shutterstock.com
Ultrasound guidance: There must be a permanent picture placed in the patient’s medical chart to meet the requirements of documentation guidelines.
- Arthrocentesis: This is the proper term for the withdrawal of fluid and/or injection of medication into a joint. If both the aspiration and injection are performed during the same encounter, only one code (20600–20611) can be used for each anatomical site.
- Insurance verification: Prior authorization for a previous procedure does not guarantee current approval. For example, the patient may have a different insurance plan. Insurance verification should be completed prior to all infusions.
- Muscles: The description of these two codes concerns the number of muscles, not the number of injections. CPT code 20552 is for one to two muscles, and 20553 is for three or more muscles. These two codes cannot be coded together. For example, if five muscles are injected, only the 20553 code can be billed, because the description states three or more muscles.
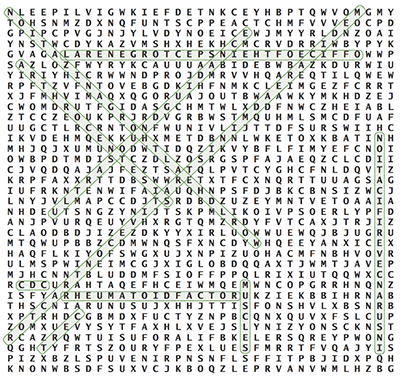
- Rheumatoid factor: This is a subcategory for rheumatoid arthritis and is the first three characters of the code.
- Office of the Inspector General: The OIG can impose civil monetary penalties and jail time, as well as provide sample compliance plans.
- World Health Organization (WHO): The International Classification of Diseases is owned by WHO. The entire world accesses the ICD codes in some manner. The U.S. uses the ICD codes for diagnosis coding and clinical medication and is currently using the 10th edition of the classification criteria.
- CDC: The Centers for Disease Control and Prevention aids WHO in maintaining and updating the ICD-10 codes. Although ICD-10 codes are used for diagnosis codes, they are also used to track mortality and morbidity data.
- Medicare Administrative Contractor: Medicare Administrative Contractors (MACs) are the different carriers Medicare contracts with to administer the claims for Medicare patients across the states and U.S. territories.
- CERT: These types of audits are used as an instrument for the Centers for Medicare and Medicaid Services to ascertain if MACs are processing claims correctly.
For questions or additional information on coding and documentation guidelines, contact Melesia Tillman, CPC-I, CPC, CRHC, CHA, via email at [email protected] or call 404-633-3777 x820.
