- A practice receives an overpayment request from the Centers for Medicare & Medicaid Services (CMS) for not meeting medical necessity related to a biologic infusion. In which instructional guideline can the coding and billing staff find the necessary information on the CMS website to handle this request?
- Internet-only manuals
- National Correct Coding Initiative
- Medically Unlikely Edits
- None of the above
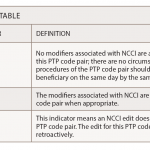
- What does the coding edit modifier indicator “0” mean on the National Correct Coding Initiative Procedure to Procedure table?
- Allowed
- Not allowed
- Not allowed unless with a modifier
- Not applicable
- What edit modifier will allow modifier -59 to bypass the National Correct Coding Initiative edit methodology to allow a claim to be processed when reported with another code?
- When the table has it listed as “0”
- When the table has it listed as “1”
- When the table has it listed as “9”
- None of the above
- When will a Medically Unlikely Edits error occur with a service/procedure?
- Removing a gallbladder that has already removed
- Giving a male a hysterectomy
- Billing for the nursing service and an infusion
- All of the above
- Providers and their office staff will always find medical policies for all Medicare Administrative Carriers in one place on the CMS website
- True
- False