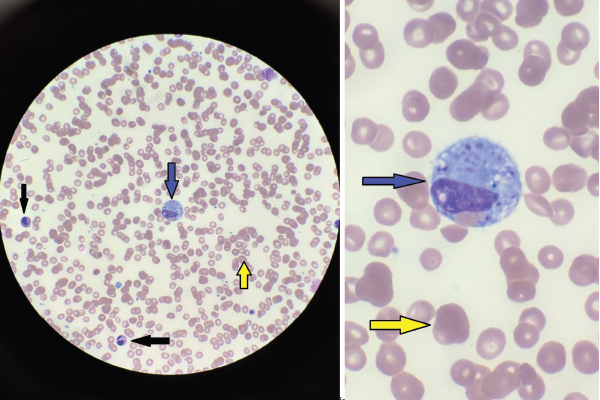
Figures 1A & 1B
Figures A (left; 40x magnification) and B right; (100x magnification). The bone marrow aspiration smear shows activated macrophages with phagocytosis of hematopoietic cells (blue arrow), including mature red blood cells (yellow arrows) and neutrophils (black arrows).
HLH probability score (H score), a freely available online calculator, was based on a multicenter, retrospective cohort of adult patients and can be used to calculate the diagnostic likelihood of HLH in patients with a constellation of clinical and laboratory features suggestive of HLH.8
The treatment of HLH in adults is derived from HLH-94 protocols developed for children and includes corticosteroids, etoposide, cyclosporin A and intrathecal therapy for patients with central nervous system (CNS) involvement.11 For patients with MAS, in contrast to other patients with secondary HLH, pulse-dose methylprednisolone (1 g/day) is the first-line treatment.
For patients who do not respond to high-dose steroids, the addition of cyclosporine at a dose of 2–7 mg/kg/day is recommended. For patients refractory to both steroids and cyclosporine, treatment protocols including etoposide should be considered.9 In our case, etoposide was started under the direction of the hematology team and the patient had a good response.
Alternative treatments for patients with MAS include intravenous immunoglobulin (IVIG), plasma exchange, cyclophosphamide and biologic agents, such as IL-1 inhibitors.9,11 Hematopoietic cell transplant (HCT) should be considered for patients with familial orgenetic mutations for HLH, underlying hematologic malignancies and CNS involvement.11
Secondary infection due to iatrogenic depletion of leukocytes is a major cause of mortality in adults with HLH. Patients being treated with HLH-specific therapies should receive intensive nursing care, neutropenic precautions and prophylaxis against opportunistic infections.11
Primary HLH, including familial HLH (autosomal recessive mutations) & lymphoproliferative syndromes, is caused by genetic mutations impairing the function of NK & T cells. Secondary HLH is usually triggered by an underlying condition.
Conclusion
HLH is rare in adults and associated with very high mortality rates, especially if associated with malignancy. A high index of suspicion in patients with symptoms of unexplained SIRS, multiple organ dysfunction syndrome and laboratory abnormalities is essential to reduce mortality. A very important indicator is a discordance between ESR and CRP and, as in our case, should raise suspicion of HLH. Prompt treatment can result in good outcomes for patients with this life-threatening disease—as in our case.
 Srujana Pachigolla, MD, is a board-certified internist and hospitalist for Carilion Roanoke Memorial Hospital, Va.
Srujana Pachigolla, MD, is a board-certified internist and hospitalist for Carilion Roanoke Memorial Hospital, Va.