
Image Credit: CLIPAREA | Custom media/shutterstock.com
Recent updates to criteria used for diagnosing neuromyelitis optica (NMO) are aimed at helping physicians make the differential diagnosis of this disorder differentiating it from other inflammatory disorders—a diagnosis that can be difficult given the presenting symptoms that can mimic a number of other conditions, such as multiple sclerosis.
Published in July 2015, the new diagnostic criteria are the result of an international consensus group comprising 18 members from nine countries and co-chaired by two investigators from the Mayo Clinic.1
According to Dean Wingerchuk, MD, professor of neurology, Mayo Clinic, Scottsdale, Ariz., one of the co-chairs, the criteria were revised from the 2006 criteria to “catch up with scientific advances and align the criteria with contemporary neurological practice.”2

Dr. Wingerchuk
One specific advance has been improvement in detecting the antibody associated with the disorder—the antibody that targets aquaporin-4 (AQP4-IgG). “This antibody is highly specific,” says Dr. Wingerchuk, “so it has helped us identify a number of clinical and radiologic patterns that fall under that umbrella of neuromyelitis optica spectrum disorders (NMOSD) that weren’t previously recognized.”
The umbrella of NMOSD that Dr. Wingerchuk refers to is one of the main new changes in the update. It provides a new nomenclature to unify the terms NMO and NMOSD, with further stratification based on the presence or absence of the antibody (i.e., NMOSD with or without AQP4-IgG).
A second important change in the updated criteria is providing a way to facilitate an earlier and accurate diagnosis of NMOSD.
Facilitate Earlier & Accurate Diagnosis
Under the new criteria, neuromyelitis optica, which is an inflammatory central nervous system (CNS) syndrome, is diagnosed in patients who are AQP4-IgG seropositive with either transverse myelitis or optic neuritis. Prior diagnostic criteria required both conditions to make the diagnosis of NMOSD.
(click for larger image)
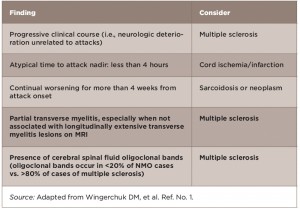
Table 1: Red Flags: Findings Atypical for NMOSD Based on Clinical & Laboratory Findings
The new criteria also identify NMOSD in patients who may present with CNS involvement beyond the optic nerves and spinal cord, and who are seropositive.
“Now, when a patient has a single attack that is consistent with an NMO spectrum disorder, and they are serum positive for the antibody, we can confirm that they have NMOSD,” says Dr. Wingerchuk.
For patients who are antibody negative, the panel provides what it calls “red flags” to guide physicians in making the differential diagnosis of NMOSD (see Tables 1–3).


