Tupungato; Svetlana Voronova/shutterstock.com
The levels of service within an evaluation and management (E/M) visit are based on the documentation of key components, which include history, physical examination and medical decision making. The history component is comparable to telling a story and should include a beginning and some form of development to adequately describe the patient’s presenting problem.
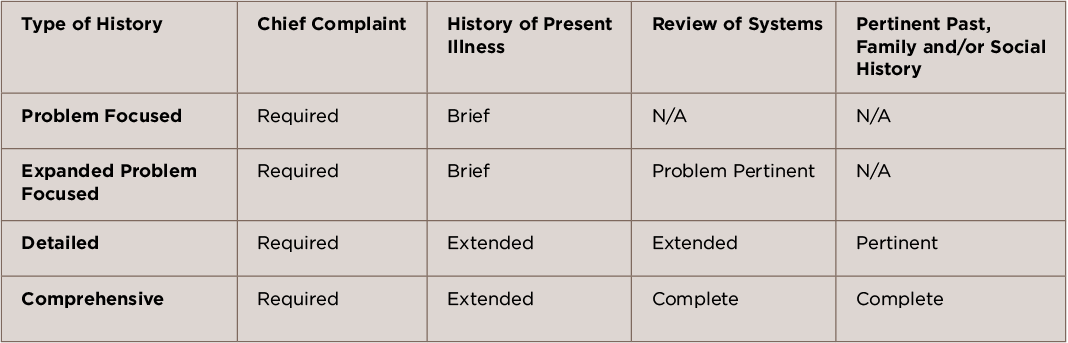
To ensure high-quality patient care and proper reimbursement, it is important that documentation of the history element tell the complete story of why the patient is in the office. The Centers for Medicare and Medicaid Services (CMS) Documentation Guidelines for Evaluation and Management Services have four history levels, each of which comprises four elements.1 To qualify for a given history level, certain elements are required, as depicted in Table 1.
Note from the table that as the type of history becomes more intensive, the elements required to perform that type of history also increase in intensity. For example, a problem-focused history requires documentation of the chief complaint (CC) and a brief history of present illness (HPI), while a detailed history requires the documentation of a CC, an extended HPI, plus an extended review of systems (ROS) and pertinent past, family and/or social history (PFSH).
Elements of History
Each type of history includes some or all of the following elements: CC, HPI, ROS and PFSH.
Chief Complaint: The patient encounter must include documentation of a clearly defined CC. Although it may be separate from the HPI and the review of systems, it must make the reason for the visit obvious, because it is the patient’s presenting problem. “Follow-up” does not constitute a chief complaint. A chief complaint should comprise a concise statement describing the symptom, problem, condition, diagnosis, physician-recommended return or other factors that establish the reason for the encounter in the patient’s own words (e.g., aching joints, rheumatoid arthritis, gout, fatigue, etc.). If a clear CC is not documented, the provider may be subject to a denial in the event of an audit and is usually referenced as not being medically necessity.
History of Present Illness: The HPI is a chronological description of the patient’s symptoms or clinical problems from the onset and/or how it has developed. HPI includes information obtained from the patient and must be obtained by the provider or a qualified healthcare professional. Some Medicare carriers have established their own policies that require the provider to perform the work of the HPI. Although interpretations of these policies may differ, the ACR recommends that practices review their contractor policies to avoid scrutiny.