Earlier studies demonstrate that inflammation may be present in a given joint even in the absence of symptoms or signs of inflammation. Also, initiation of therapy early in RA is more effective than treating longstanding disease. The greater the burden of disease as evidenced by radiographic joint damage at the onset of therapy, the more likely the disease will be progressive and resistant to therapy. These observations suggest that an additional mechanism may become engaged once joint damage has occurred, which is capable of stoking the flames of inflammation, resulting in even greater disease burden. In addition to a potential role in the initiation of the disease, TLRs may contribute to disease progression.
TLRs in the RA Joint
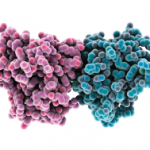
For TLRs to promote inflammation in RA, not only must they be present and functional at the site of inflammation, but TLR ligands must be available locally that are capable of activating through the TLR signaling pathway. Although synovial fibroblasts express TLRs and respond to TLR ligands, cells of the innate immune system, such as macrophages and dendritic cells, are more important for their TLR-mediated responses. We demonstrated that TLR2 and TLR4 on macrophages isolated from the joints of patients with RA are increased compared with their expression on control peripheral blood monocytes or control in vitro differentiated macrophages or macrophages isolated from the joints of patients with other forms of inflammatory arthritis, such as psoriatic arthritis and ankylosing spondylitis.22 In addition, RA synovial fluid macrophages demonstrate a significantly increased response to the TLR2 microbial ligand peptidoglycan and the TLR4 microbial ligand LPS compared to control peripheral blood monocytes or monocyte in vitro differentiated macrophages and macrophages from the joints of patients with psoriatic arthritis and ankylosing spondylitis. This increased sensitivity to signaling though the TLR pathway, which may be mediated through decreased production of the antiinflammatory cytokine IL-10 or increased production of the proinflammatory cytokine interferon γ, may contribute to the progressive inflammation and joint destruction that may be seen in RA, and it may prime patients for progressive inflammation and destruction by RA. It is interesting to speculate that disease-associated TNFAIP3 SNPs might also contribute to this increased TLR-mediated activation in some patients.
Endogenous TLR Ligands in the RA Joint
What are the potential TLR ligands that might drive the chronic inflammation and joint destruction observed in patients with RA? For TLR2 and TLR4 ligands to be active, they must gain access to the extracellular space within the joint, which may be sampled in part by the analysis of synovial fluid. A variety of putative TLR ligands have been described based on their ability to activate through the TLR signaling pathway, including molecules such as HSP-60, -70, and -22, EDA fibronectin, and the structural molecule biglycan. However, we were unable to identify HSP-60 and -70 or biglycan extracellularly in RA synovial fluid and very low endotoxin HSP-60, -70 and -22 failed to activate through TLR2 or 4.23 Further, endotoxin is a contaminant that is capable of activating through TLR4 when recombinant proteins are expressed in Escherichia coli. Therefore, any study that employs recombinant proteins to identify their ability to serve as TLR ligands must take this concern into account.