Screening & Monitoring for ILD
To help with screening decisions, the first guideline provides a detailed list of disease-specific factors that may increase a patient’s risk of developing ILD, drawing on elements from a patient’s medical history, current presentation and laboratory results.1 Patients who lack the risk factors and are asymptomatic may not necessarily need screening beyond their regular history and physical exam (see Figure 1).
“If clinicians are uncertain whether a patient should be screened or not, they should err on the side of caution and screen,” says Dr. Johnson.
One recommendation: Pulmonary function tests (PFTs) are conditionally recommended over history and physical exam or ambulatory desaturation testing alone to screen for ILD in SARD patients at higher risk.
Others conditional recommendations are for high-resolution computed tomography (HRCT) of the chest over PFTs alone, and for HRCT over history and physical exam, as well as in favor of chest HRCT with PFTs over PFTs alone.
Dr. Bernstein has a strong preference for screening all people who have SSc with HRCT at presentation, due to the high prevalence of the disease in this population and the fact that PFTs alone may miss early ILD.
The Patient Panel expressed a strong preference for early diagnosis of ILD, even if more frequent screening leads to identification of subclinical disease or incidental findings that may require further testing.
Once diagnosed with ILD, SARD patients require monitoring for their response to therapy, typically in conjunction with pulmonology. The Patient Panel strongly preferred more frequent testing over less frequent testing to avoid missing signs of progression.
Treatment of ILD in SARDs
Most recommendations in the treatment guideline were based on low or very low certainty of evidence, as were the recommendations on screening and monitoring treatment. Dr. Johnson points out that in these circumstances, patients’ preferences and values more strongly influence treatment choice. “The Patient Panel told us they wanted clear communication about the advantages and side effects [of therapies], so they could be actively involved in their choice of medication,” she says.
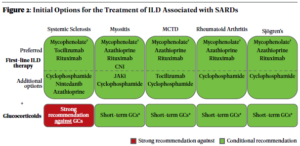
The guideline recommendations are stratified by first-line treatments (see Figure 2) vs. treatments to consider if a patient’s disease has progressed after initial treatment, with certain recommendations specific to individual SARDs (see Figure 3). Additional recommendations clarify additional treatment approaches in patients with rapidly progressing disease (see Figure 4).